Login
Heart and Vascular Programs
Center for Aortic Health
With the right care, you can count on a healthy aorta.
Why Choose ChristianaCare?
You probably haven’t given a lot of thought to your aorta. It’s the largest artery in your body and it can develop certain problems, some very serious. With the right care, you can count on a healthy aorta. Having your usual physician connected with a specialty team focused on aortic health means you’ll get the right care. And if a problem does develop, you’ll know you have experts you can trust to help.
At ChristianaCare, we’ve assembled a team dedicated to helping you keep your aorta healthy. The expertise of specialist physicians, surgeons and radiologists are brought together to be sure you and your primary care doctor have the best health maintenance advice, and they’re ready to help with any aortic problems you might experience. Medications, surgeries and less invasive endograft procedures (more on that below) can all be part of a care plan.
Maintaining Aortic Health
Chances are you’ve never thought much about your aorta, but common conditions can cause your aorta trouble. High blood pressure, high cholesterol, cigarette smoking and a family history of aortic or other blood vessel problems can put you at higher risk of aortic disease. Untreated, aortic disease can lead to serious problems including life-threatening emergencies.
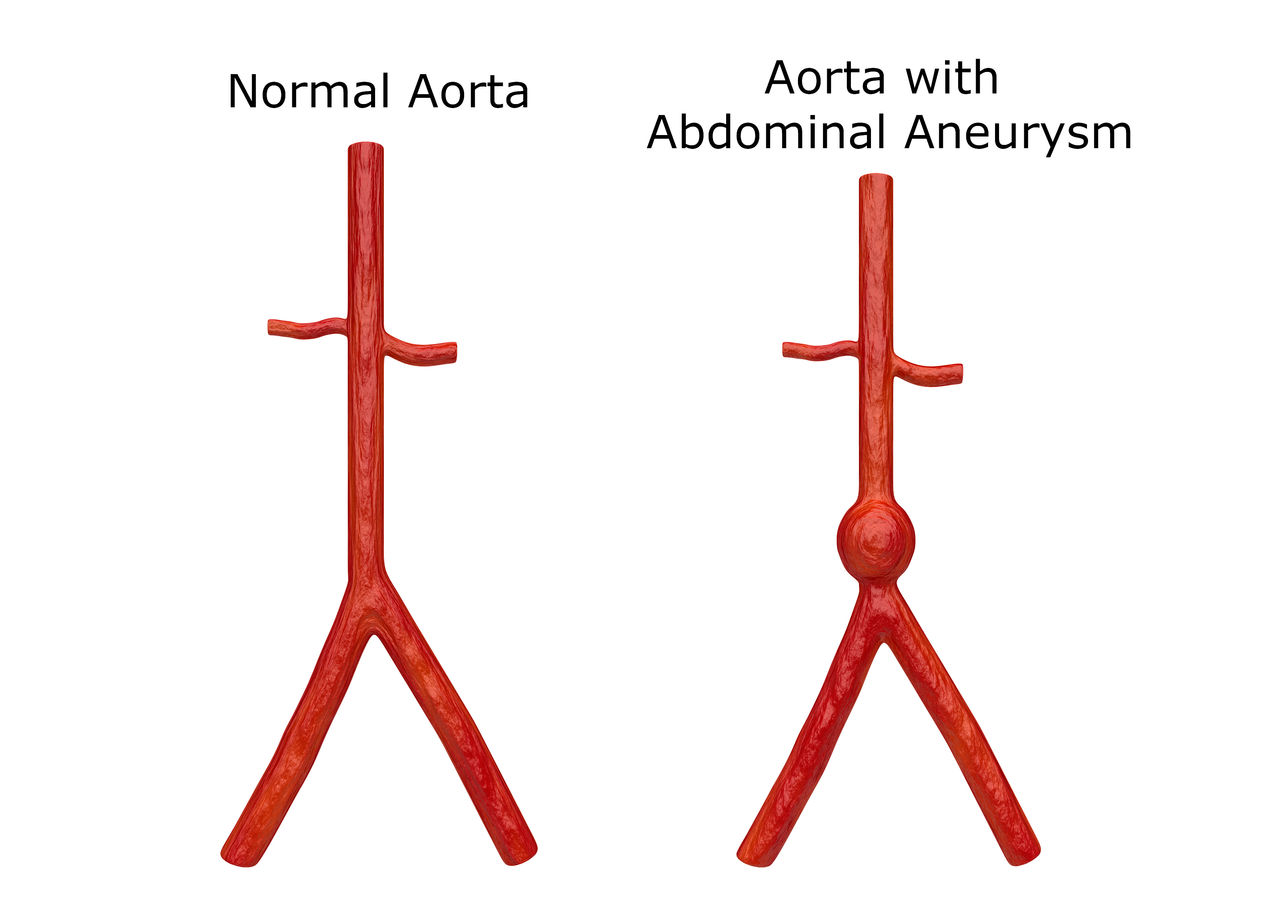
Your aorta connects to the top of your heart and carries oxygen-rich blood from your heart to the rest of your body. This large blood vessel travels from your chest and into your belly, giving off many branches. Problems can be limited to the chest (thoracic), the belly (abdominal) or both parts of the aorta (thoracoabdominal).
Frequently Asked Questions
If you’ve never had any aortic problem, your primary care physician (PCP) can handle everything. The ChristianaCare Center for Aortic Health makes it easy for your providers to get advice or help from a specialist if needed. If you have an aortic problem diagnosed, chances are good that you’ll be referred to a specialist. This is often a cardiologist but could be a vascular surgeon, cardiac surgeon or even a vascular radiologist.
Your doctors will let you know if surgery is necessary to fix an aortic aneurysm. Some aneurysms can be managed without surgery or followed for a time before surgery becomes necessary. Your doctors are likely to consider surgery once an aneurysm grows above 2 inches or so in diameter because catastrophic dissections and ruptures are more likely when the diameter gets much bigger than that. The speed at which the aneurysm grows is also a factor: doctors usually advise surgery if an aneurysm grows more than about one half-inch in a year. Medications can help slow the growth of an aneurysm. Today, many aneurysms can be treated with endograft methods (see below).
With regular surgery and endograft treatment, synthetic material is used to reinforce or replace parts of the aorta. The materials used have been used for vascular repairs for many years and are both safe and effective.
Unlike aneurysms, dissections tend to happen suddenly and cause a lot of symptoms. Generally, a CT scan can tell your doctors if you have a dissection. If you do, the care you’ll need will depend on the location and extent of the dissection.
Remember that the thoracic part of your aorta starts at the top of your heart and runs toward your head. That first part is called the ascending thoracic aorta. It then turns 180 degrees and runs through your chest toward your belly. The turning part is called the aortic arch (or transverse arch) and the rest is called the descending thoracic aorta.
Dissections involving the ascending thoracic aorta or the aortic arch can be very dangerous. Emergency surgery may be necessary to prevent permanent injury or death. Dissections in the ascending thoracic aorta can interfere with the function of the aortic valve, a major heart valve, and replacing that valve is sometimes necessary. On the other hand, some dissections that involve just the descending thoracic aorta can be managed with medications alone. Other dissections can be treated with endograft techniques, especially those limited to the abdominal aorta. If a dissection involves both the thoracic and abdominal parts of the aorta, surgery might involve operating on both the chest and the abdomen, or a combination of surgery and endograft techniques may be needed.
Aortic operations are major surgeries. Sometimes a combined team of cardiac and vascular surgeons needs to work together to bring about the best results possible. We take this team approach at the ChristianaCare Center for Aortic Health.
Endografts are large tubes (sometimes called stent grafts) that can be placed inside your aorta to treat some aneurysms and dissections. Typically, they’re inserted through an incision in the groin. Endografts are attractive because they’re a less stressful alternative to surgery, and they generally have fewer complications than surgery. However, some aneurysms and dissections are not suitable for treatment with endografts.
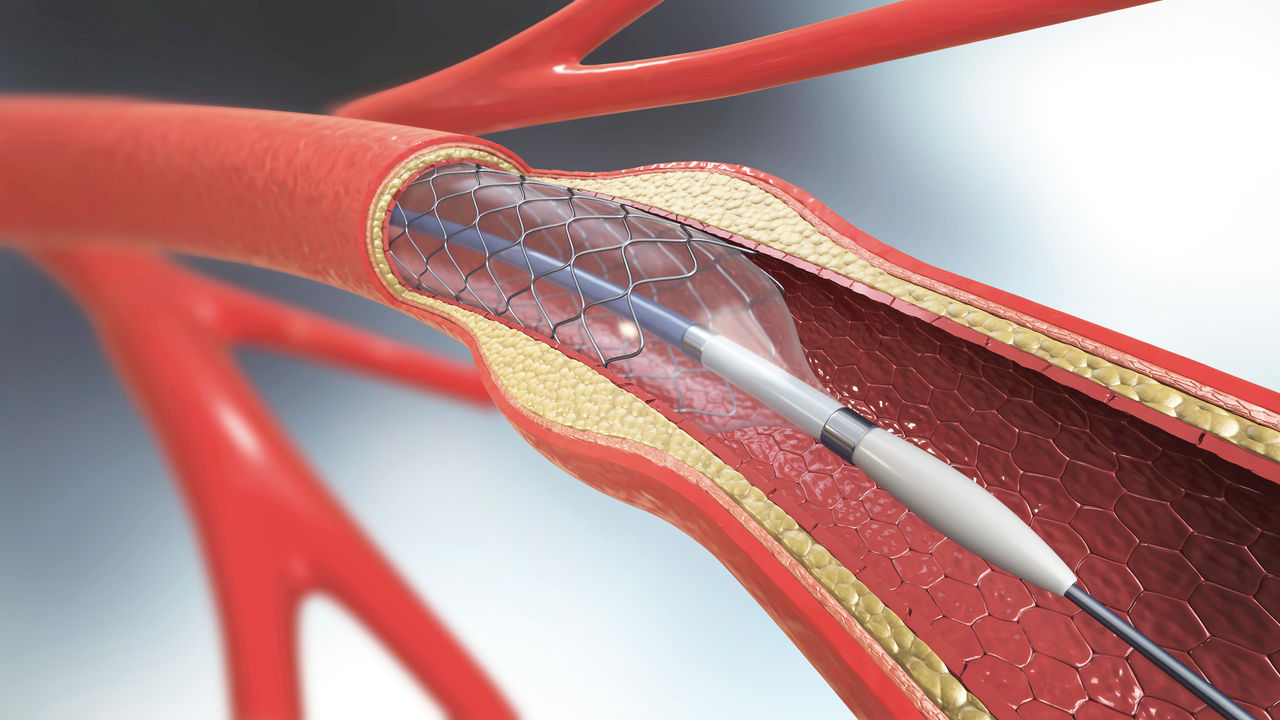
The most common use of endografts is in the treatment of abdominal aorta aneurysms, where they’ve proven very helpful. Endografts can effectively cover and seal off an aneurysm. Care is required to assure the endograft doesn’t cover important blood vessels branching off the aorta, like the arteries going to kidneys and other organs.
Endografts have also been used to treat aneurysms in the descending thoracic aorta. The greatest concern here is that small blood vessels branching from the descending thoracic aorta provide blood to the spinal cord, and covering them can lead to nerve weakness or paralysis. Endografts are being developed for use in the ascending thoracic and arch aortic portions, but these are still mostly experimental.
Endografts can be used to treat aortic dissections, too, especially in the descending thoracic and abdominal aorta. Dissections in these parts of the aorta often settle down with medical therapies alone, so endografts are generally recommended when the dissections are causing trouble despite medical treatment or there’s reason to believe the dissections may cause catastrophic complications.
The downside to endografts it that they can leak. CT scans are usually done every year after an endograft to be sure it’s working properly. If an endograft leaks, you might need additional endograft treatment or even surgery.
Cardiac surgeons, vascular surgeons, interventional radiologists and cardiologists may be trained in use of endografts. At ChristianaCare’s Center for Aortic Health, we rely on the combined expertise of all these specialists to deliver coordinated care.
As with other complicated medical issues, you should discuss care of any aortic problem with care providers you trust. Most patients and care providers want to use the least invasive, least stressful approach to treat an aortic problem. However, many factors must be considered, and you should depend on the advice you get from your care team about what treatment is best for you. That’s why it’s so important to rely on providers you trust. Having a multi-disciplinary team of experts review your problem is likely to produce the best recommendation – that’s why we use this approach at ChristianaCare.
Related Content
Contact Us
Christiana Hospital
4755 Ogletown-Stanton Road,
Newark, DE 19718