Login
Stroke Program
Stroke Warning Signs
Warning signs of a stroke mean your brain is not getting enough oxygen.
If you experience any of these symptoms, do not delay. Call 911 immediately!
Warning signs of a stroke are clues that your brain is not getting enough oxygen. You and your family should learn these warning signs. You could have only one, or you may have several. They may last only a few minutes. You can help lower your risk of death or disability by knowing these warning signs.
If you suspect a stroke, do the BE FAST test to recognize the symptoms
Time lost is brain lost; with every minute that goes by, brain cells die. There are treatments which can be started in the hospital to open up a blocked artery in the brain but they need to be started as soon as possible. One is a medication called alteplase, but it can only be given within a few hours of the start of stroke symptoms. There are other treatments including emergency surgeries to open up blocked blood vessels; these treatments must be started as soon as possible as well.
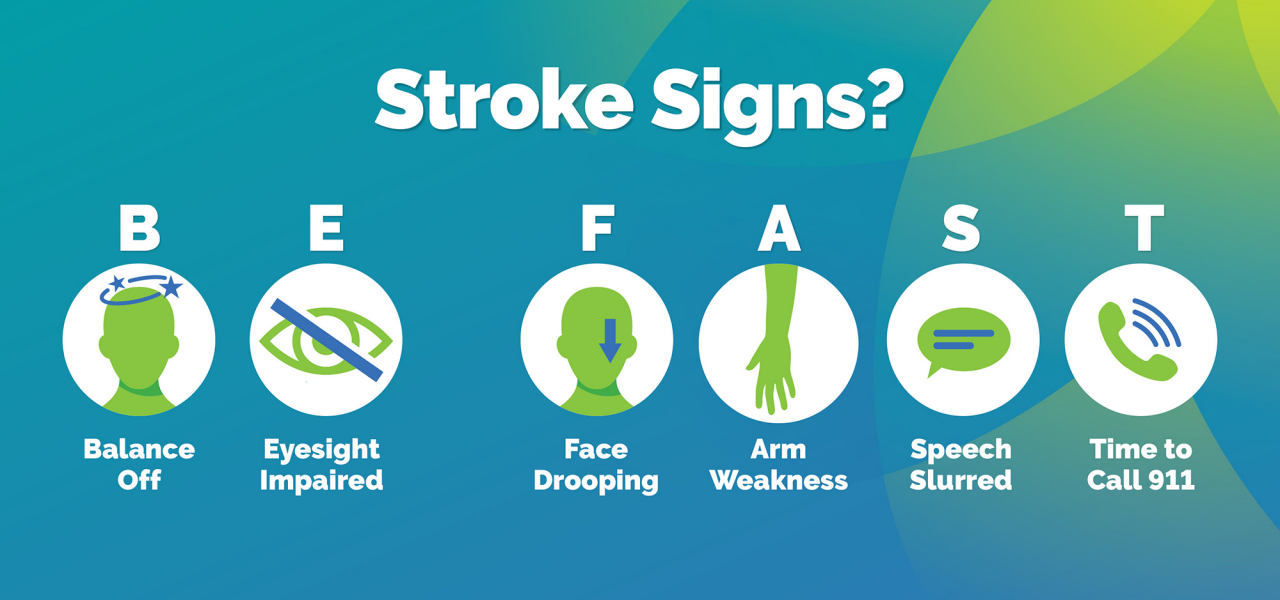
Learn what BE FAST means to know the stroke warning signs.



.png/_jcr_content/renditions/cq5dam.thumbnail.319.319.png)