Login
Model of Care
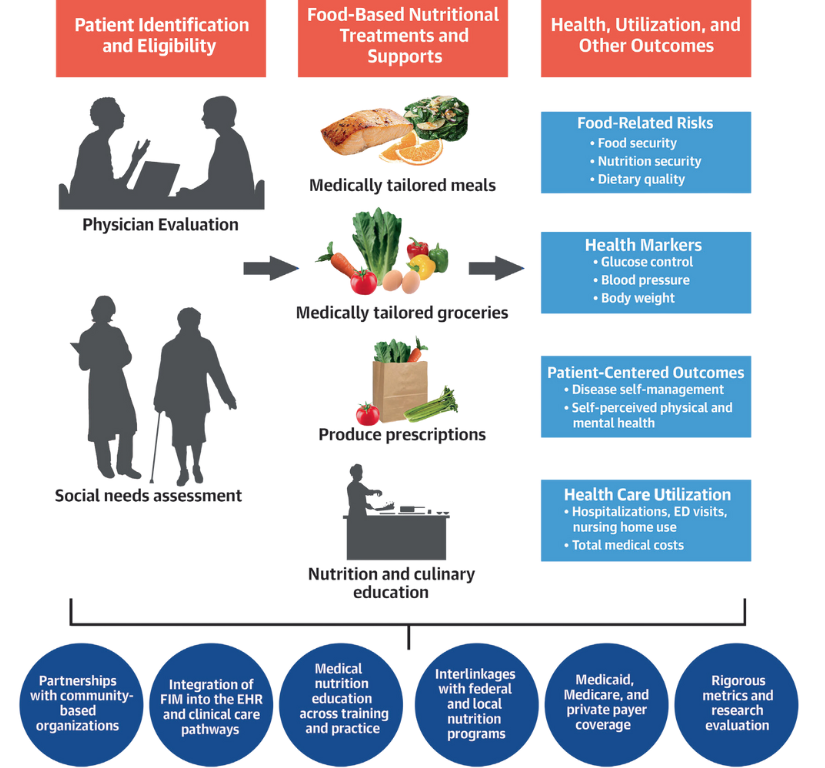
At ChristianaCare, we are advancing a model of care that recognizes food as a powerful tool for improving health. Through our Food is Medicine (FIM) initiatives, we integrate nutrition into clinical care pathways to help patients manage chronic conditions, reduce hospital utilization, and support long-term wellness.
As a trusted healthcare provider rooted in community, we’re building a system where nourishing food is formally incorporated into treatment planning—right alongside medications and therapies. By addressing the root causes of illness, including food insecurity and poor nutrition, ChristianaCare is helping lead the shift from reactive care to proactive prevention.
Through Food is Medicine, we are working to ensure every patient has access to the resources, support, and nourishment they need to thrive.
What is "Food is Medicine"?
“Food is medicine” is the provision of healthy food to prevent, manage, or treat specific clinical conditions in a way that is integrated within the healthcare sector. Patients are referred to these services by a healthcare provider, healthcare organization, or health insurance plan. Preliminary evidence indicates that delivering food is medicine programs may improve health outcomes, reduce healthcare utilization and costs, address health disparities, and reduce nutrition and food insecurity for patients living with acute or chronic diseases.
— American Heart Association: Health Care by Food
At ChristianaCare, we embrace this approach as a vital extension of our commitment to whole-person care. Food is Medicine interventions connect patients with medically supportive foods and nutrition education through clinical pathways—making food a formal part of the treatment plan, just like prescribing medications or therapies.
Our programs are delivered through partnerships between clinical teams, community organizations, and Registered Dietitian Nutritionists (RDNs). These services include:
 Mozaffarian D, et al. J Am Coll Cardiol. 2024;83(8):843–864
Mozaffarian D, et al. J Am Coll Cardiol. 2024;83(8):843–864
- Medically tailored groceries
- Produce prescription programs
- Culturally responsive nutrition education
By integrating nutrition into care delivery, we are advancing a model where food supports healing, strengthens chronic disease management, improves quality of life, and reduces disparities for the communities we serve.
Why "Food is Medicine" is Important
Poor nutrition is the leading driver of death and disability in the United States. Diet-related chronic diseases—such as diabetes, hypertension, heart disease, and obesity—disproportionately affect individuals with lower incomes, those living in rural areas, and historically marginalized racial and ethnic communities.
Despite these realities, nutrition remains largely underemphasized in the healthcare system, fueling the continued rise of preventable disease, escalating costs, and deepening health inequities.
The statistics are stark:
- 1 in 2 U.S. adults has diabetes or prediabetes
- 3 in 4 adults have overweight or obesity
- 4 in 15 adults have suboptimal cardiometabolic health
Among teenagers, the pattern is equally alarming: one in four has prediabetes, one in four has overweight or obesity, and one in eight is living with fatty liver disease—conditions that were once rare in youth and now signal a troubling public health trend.
Each year, poor diets are linked to more than 500,000 deaths—largely due to insufficient intake of fruits, vegetables, nuts, whole grains, seafood, and healthy fats, alongside excessive consumption of salt, processed meats, and sugary beverages.
The economic toll of diet-related illness is immense. Combined healthcare spending and lost productivity due to poor nutrition costs the U.S. economy an estimated $1.1 trillion annually—approximately equal to the total economic output of the entire U.S. food industry.
- About 85% of healthcare expenditures are tied to treating chronic conditions driven by poor diets.
- Diabetes alone accounts for $237 billion in direct medical expenses each year, plus another $90 billion in lost workplace productivity—together exceeding the combined budgets of the USDA, NIH, CDC, and FDA.
Many of these conditions are preventable. Food is Medicine interventions offer a high-impact, cost-effective solution. For example:
- Expanding access to medically tailored meals could save the healthcare system an estimated $13.6 billion per year, even after accounting for program costs.
- Produce Prescription programs demonstrate cost-effectiveness comparable to clinical standards like blood pressure or cholesterol management.
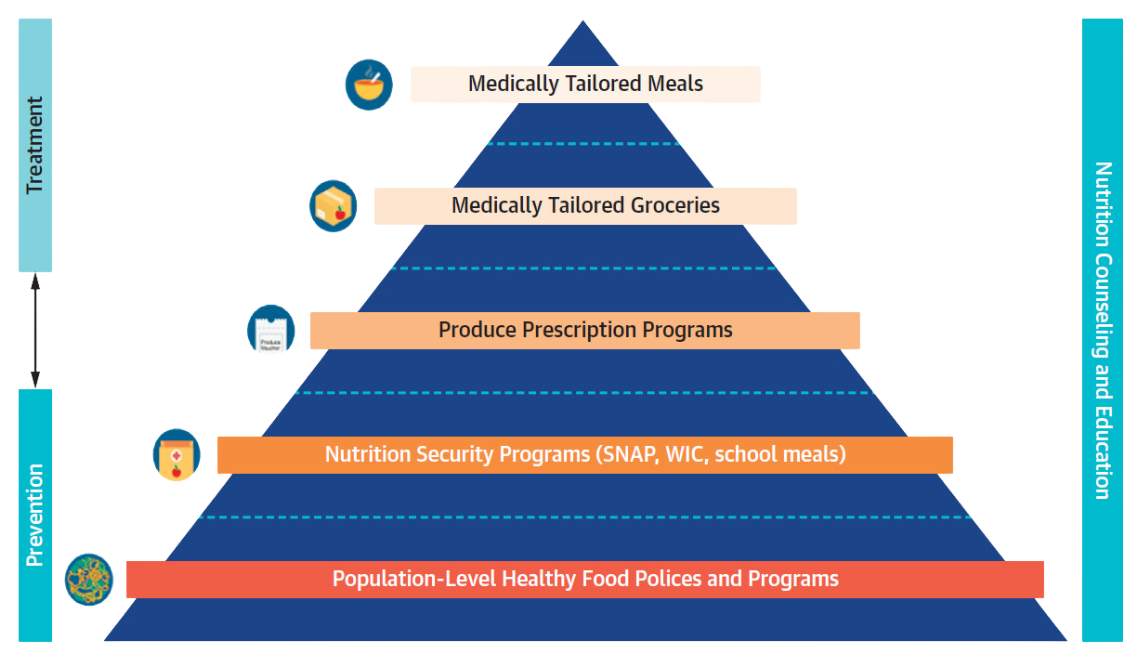 The FIM Pyramid (Source: https://www.nature.com/articles/s41591-022-02027-3)
The FIM Pyramid (Source: https://www.nature.com/articles/s41591-022-02027-3)
Food is Medicine Approaches
Food is Medicine interventions take multiple forms, each tailored to meet the nutritional and medical needs of patients based on their health conditions, lifestyles, and level of support required. These approaches are clinically integrated and often prescribed as part of a treatment plan by healthcare providers.
Medically Tailored Meals (MTMs)
MTMs are fully prepared, home-delivered meals designed by Registered Dietitian Nutritionists (RDNs) to meet the specific nutritional needs of individuals with serious or chronic health conditions. These meals are ideal for patients who are unable to shop or cook for themselves due to illness or recovery. In addition to addressing food insecurity, MTMs offer targeted dietary support during critical periods of care.

Medically Tailored Groceries (MTGs)
MTGs are curated grocery packages that include nutrient-dense foods such as fruits, vegetables, whole grains, lean proteins, dairy, and legumes. They are prescribed based on a clinical diagnosis and intended for patients who are able to cook but require support in accessing and affording medically appropriate foods. MTGs are often sourced through partnerships with community organizations, ensuring culturally appropriate and high-quality ingredients.

Produce Prescription Programs (Produce Rx)
These programs allow healthcare providers to “prescribe” fresh fruits, vegetables, and other healthy foods to patients through vouchers, coupons, or electronic benefits. Prescriptions can be redeemed at participating retailers such as grocery stores, farmers markets, and online grocers. Produce prescriptions are often paired with nutrition education and wraparound services to support long-term dietary change and improve nutrition security—particularly for patients managing diet-related chronic diseases.

Programs and Resources
Culinary Medicine
Culinary Medicine combines the art of cooking with the science of medicine to help individuals make informed decisions about their dietary habits.
Delaware Food Farmacy
This program aims to improve food access, dietary behaviors, chronic disease management, and overall health outcomes while reducing hospital utilization.
Farm to Pharmacy
The Farm to Pharmacy program integrates food access seamlessly into a familiar, trusted healthcare touchpoint—a community pharmacy.
Healthy Food Prescriptions
A six-month initiative designed to help ChristianaCare patients better manage chronic conditions through improved nutrition and food access.
Resources
Learn more about Food is Medicine impact as well as our partners, memberships and affiliations
Related Content
Contact Us
For questions please email Michelle.Axe@ChristianaCare.org


