Login
Insights & Innovations
The latest advancements, breakthroughs, and experience perspectives
About Insights & Innovations
General Surgery
Without proper care, chronic wounds can lead to serious complications, including infection, amputation and prolonged disability. At ChristianaCare’s Wound Care & Hyperbaric Medicine Center, specialists use advanced technologies and hyperbaric oxygen therapy to help patients heal.
“The Wound Care Center is a place where we utilize our expertise to focus on healing wounds,” said James Ley, M.D., a wound care and infectious diseases specialist at ChristianaCare. “We have a variety of specialized products for wounds available to us. We are very careful to establish a clear-cut etiology for a wound, and we try to address any obstacles to healing.”
Patients with wounds may initially present to their primary care doctor, who may not have the resources or equipment to adequately support healing. The Center is a specialized resource to meet patients’ needs when routine care is not enough, and we have fairly tight protocols. We see patients on a regular basis, we used an advanced technology to measure wounds and determine the composition of tissue in the wound, to know patients healing progress. Our goal is to heal all of our wounds within 12 weeks or so.”
The Wound Care Center treats a wide range of conditions, including venous stasis ulcers, diabetic foot ulcers, pressure injuries and complex traumatic wounds. Dr. Ley recommends referral for wounds that don’t heal within 30 days of routine care or have the potential to become chronic.
Treatment at the Wound Care Center is highly individualized to identify and remedy underlying causes and barriers to healing. The Center deploys specialized wound care products, from dressings that manage drainage, to collagen-based products that promote tissue growth, to antimicrobial dressings that protect against infection.
In addition, Cellular tissue products (CTP’S) are a biological or synthetic material used to treat wounds, especially those that are difficult to heal, by mimicking the structure and function of human skin. These products can be derived from human or animal sources and may contain viable or non-viable cells. They are designed to promote wound closure, reduce inflammation and improve tissue regeneration, and they represent some of the newest innovations in wound care technology.
“We continue to utilize new products as they become available if we think they will give us an advantage,” Dr. Ley said.
Patients treated at ChristianaCare also have access to hyperbaric oxygen therapy. This treatment places patients in pressurized chambers where they receive 100% oxygen. This high pressure forces oxygen to dissolve into the blood, allowing increased delivery to tissues where it promotes healing, reduces inflammation and helps fight infection.
The therapy is particularly effective for radiation-induced injuries, including radiation cystitis or delayed wound healing in patients who have received radiation treatment for breast or prostate cancer. Patients with radiation damage to the jaw, teeth or mouth tissues from treatment for head and neck cancer also benefit significantly from hyperbaric oxygen treatment.
“We’re able to apply hyperbaric oxygen therapy to those situations, and we see fairly good results,” Dr. Ley said. “We’ve seen function improve significantly, where people are hardly able to eat, but after treatment, can actually begin to eat again and chew food.”
ChristianaCare’s Wound Care Center uses a multidisciplinary approach to wound healing, with access to many specialists in vascular surgery, plastic surgery, general surgery, podiatry and infectious disease. This comprehensive team ensures that the underlying causes of wounds are properly addressed, not just the surface symptoms, so patients can heal quickly.
“In our area, we’re the main provider for this kind of care,” Dr. Ley said. “We have a lot of depth in being able to deal with the underlying causes of wounds.”
The recent addition of a hybrid OR suite at the ChristianaCare Center for Heart and Vascular Health has enabled surgeons to transform the care offered to patients with complex cases, allowing for surgeries that just months ago wouldn’t have been possible.
The room—housed within the Gerret and Tatiana Copeland Heart and Vascular Interventional Suites—features built-in capabilities for x-ray, fluoroscopy and CT scans, and it enables procedures that combine traditional open surgery and minimally invasive techniques.
“It’s very advanced equipment that allows us to do things that we couldn’t do before,” said Kathryn Bowser, M.D., a vascular surgeon and one of the founding physicians of the ChristianaCare Center for Aortic Health. “It allows us to treat some extremely complex disease processes.”
“Without a doubt, the suite allows us to do procedures that would not have been a possibility before,” added vascular surgeon Mikael Fadoul, M.D. “The integrated fusion technology has really enhanced our ability to treat complex aortic pathology, specifically thoracoabdominal aneurysms.”
Since opening in February 2025, the room has been used regularly to treat advanced aortic disease that sometimes used to require transfer to other facilities, such as aortic aneurysms, aortic thrombus and aortic dissection.
“These procedures may have previously required patients to be transferred out of the hospital, or had to be done purely with open surgery,” said Dr. Bowser, who is also site primary investigator for the recently funded multi-institutional trial called WARRIORS, or Women’s Aneurysm Research: Repair Immediately or Routine Surveillance. “Now, if we can do them in a less invasive manner with this advanced technology, we can provide much better outcomes for patients. These are things that just can’t be done any other way. In another OR, you’d have to bring in additional equipment; you can’t see as well. It becomes much more cumbersome. In the new suite, everything is integrated into the room in order to allow us to do these different types of surgeries.”
“The room has allowed us to do custom fenestrated devices for patients who otherwise would not have had an option for minimally invasive repair,” Dr. Fadoul added. “There is nowhere else in the state of Delaware that is doing this, and only a handful of places on the East Coast.”
The Heart and Vascular team at ChristianaCare has also been pioneering procedures for thoracic aortic dissection that reduce the need for open thoracic surgery. In addition, the team was the first in Delaware to use a GORE EXCLUDER Thoracoabdominal Branch Endoprosthesis device, which is the first FDA-approved, off-the-shelf device for treating complex aneurysmal disease involving the visceral aorta.
Meanwhile, the health system leads the region in treatment of aortic pathology. For example, ChristianaCare was the first system in Delaware to perform thoracic branch endograft. The team has also been conducting deep vein arterialization and using innovative systems such as LimFlow and DETOUR, which are used to restore blood flow to the lower limbs in patients suffering from severe critical limb ischemia and peripheral arterial disease.
“ChristianaCare has been at the forefront of getting these technologies brought into the health system in order to allow us to provide the most up-to-date care for otherwise no-option patients,” Dr. Fadoul said.
“We can really expand care to help people in Delaware in a way we have never been able to before,” Dr. Bowser added. “And we couldn’t be doing it without access to a room like the hybrid OR suite.”
Robotic-assisted surgery offers patients precision, improved outcomes and faster recovery. The comprehensive robotic surgery program at ChristianaCare spans multiple specialties, and its experts have performed more than 20,000 operations, establishing the program as a leader in minimally invasive surgery.
The scope of robotic surgery at ChristianaCare spans general surgery, thoracic surgery, urology, colorectal surgery, obstetrics and gynecology, ENT and oncology, making it one of the region’s most comprehensive robotic surgery programs.
“Certainly, within the state of Delaware, our institution offers the widest spectrum of specialties utilizing robotics in surgery,” said Peter Santoro, M.D., Section Chief of General Surgery and Director of Robotic Surgery at ChristianaCare. “It’s a comprehensive healthcare system, where patients can receive whatever type of surgical care they need. In total, we have done, as a system, almost 21,000 robotic operations since the inception of the robotic surgery program.”
Minimally invasive techniques like robotic-assisted surgery offer significant benefits over traditional open and even laparoscopic surgical approaches. By utilizing robotics in surgery, patients experience smaller incisions, faster recovery times, a quicker return to work, reduced postoperative pain and decreased narcotic use.1,2 These advantages translate to improved patient satisfaction and better overall surgical experiences.
The precision afforded by robotics allows surgeons to perform complex procedures through small incisions, and enhanced visualization, improved dexterity and tremor filtration enable surgeons to operate accurately in confined spaces and around delicate structures.
ChristianaCare’s broad robotic surgery capabilities are facilitated by seven state-of-the-art da Vinci (DV) surgical systems. These robotic platforms are manufactured by Intuitive Surgical, a leading medical technology company that pioneered robotic-assisted minimally invasive surgery.
“Earlier this year, we added two new systems to upgrade our fleet from five robots to seven robots,” Dr. Santoro explained. The recent addition of two new DV5 systems, the newest model offered by Intuitive, is the latest advancement in ChristianaCare’s robotic service offerings.
The seven robotic systems are strategically distributed across the health system, with five Xi models at Christiana Hospital—four in the main operating rooms and one in the surgery center—and the two DV5 units at Wilmington Hospital. This distribution ensures that patients throughout the system have access to robotic surgery without geographic barriers.
“We are constantly assessing and adding technology as needed to keep our access to care as easy as possible for all patients within our system,” Dr. Santoro said.
ChristianaCare’s robotic surgery program stays at the forefront of innovation by actively evaluating new technologies and techniques, ensuring patients access to the latest surgical advances.
“This is a field that’s constantly evolving. We are always evaluating new technology. There are a lot of new companies that are developing robotic technology that will become more mainstream and utilized within healthcare systems very soon,” Dr. Santoro said. “ChristianaCare is definitely on the forefront of evaluating those systems for potential integration into our program.”
Through continued investment in technology, ongoing expansion of capabilities and commitment to surgical excellence, ChristianaCare’s robotic surgery program sets the standard for minimally invasive surgical care in the region, providing patients with the best possible outcomes through the most advanced surgical techniques available.
“ChristianaCare, as a healthcare system, is very much about expanding access for our patients,” Dr. Santoro said. “Just as we expand our capabilities, our specialists and our surgeons.”
References
- Cureus. 2024;16(2):e54433.
- J Gastrointest Surg. 2023;27(10):2057-2067.
In the field of surgical oncology, innovative techniques are transforming surgeries so patients spend less time in the hospital, recover faster and experience improved outcomes on their cancer journeys. At ChristianaCare, the surgical oncology team consists of four specialists: Leon Kushnir, M.D.; David Christopher Palange, D.O.; Arvind Sabesan, M.D.; and Brendan Hagerty, M.D. Together, they provide care for individuals with a broad range of conditions.
In general, a large portion of the practice focuses on upper GI and hepatobiliary cancers, pancreas cancer, liver cancer, stomach and small bowel cancers, and peritoneal surface cancer. In addition, Dr. Kushnir, an endocrine surgeon, specializes in thyroid, parathyroid and adrenal surgery. Dr. Palange focuses on rectal surgery—for both benign and malignant disease. As board-certified surgical oncologists, Drs. Sabesan and Hagerty treat a range of malignancies, including melanoma, sarcoma and other skin or soft tissue cancers.
Over the past year, the team focused on expanding the scope of their robotic surgery program so more patients can be treated with cutting-edge, minimally invasive techniques.
“We are working towards making our center the go-to place for minimally invasive pancreas, liver and bowel resection surgery,” Dr. Hagerty said. “This has not been done at ChristianaCare in the past, and—with few exceptions—isn’t being done elsewhere in the region.”
Within the next few months, the team will begin to offer a robotic-assisted Whipple procedure—also known as robotic-assisted pancreaticoduodenectomy—that can benefit those with complex cancers of the pancreas, duodenum and bile duct by reducing recovery time, decreasing pain and providing better outcomes than open surgery.
While it is associated with a longer operative time, robotic pancreaticoduodenectomy has been shown to generally correlate with high patient satisfaction scores and may result in better rates of survival at one year, three years and five years after surgery when compared with traditional open pancreaticoduodenectomy.1
“The ultimate goal with this program is not just to get patients out of the hospital and recovered faster, but to positively affect their overall outcomes,” Dr. Hagerty said. ““We believe this approach may mitigate post-operative complications and improve recovery which has been shown to improve cancer-related outcomes.”
For melanoma patients, Dr. Hagerty and his colleagues promote a cutting-edge technique called targeted axillary dissection, which potentially eliminates the need for more complex surgeries among those with clinical stage III disease.
“In the past, patients would have their melanoma resected and have the entire involved nodal basin resected as well—what’s called a lymphadenectomy,” Dr. Hagerty said. “More recently, we’re taking an approach where we give patients immunotherapy up front before surgery, have their nodes shrink down, and remove only the diseased nodes. We then check them for response, and tailor their approach based upon the degree of response seen in the lymph node.”
This personalized approach can essentially eliminate the need for larger surgery, decreasing morbidity and resulting in faster recovery times.
“The trials that have explored this approach have noted incredible results with excellent long-term outcomes, which were never seen in the melanoma space before,” Dr. Hagerty said.
In offering these and other innovative techniques for cancer patients, the ChristianaCare’s surgical oncology team is investing in cutting-edge care today with the goal of extending the health of patients well into the future.
“We want to benefit our patients not just in the short term, but in the long term as well,” Dr. Hagerty noted.
Reference
- Ann Gastroenterol Surg. 2021;5(5):589-596.
The ChristianaCare Oral and Maxillofacial Surgery & Hospital Dentistry department continues to expand its capabilities in both routine procedures and complex tertiary care, serving as a regional hub for comprehensive maxillofacial treatment.
The experts in the department integrate dental, medical, and surgical expertise into a single, highly specialized discipline.
“Oral and maxillofacial surgery (OMFS) is a specialty that bridges medicine, dentistry and surgery all together,” said Daniel Meara, M.D., D.M.D., the chair of ChristianaCare’s Department of Oral and Maxillofacial Surgery & Hospital Dentistry. “Our gamut is everything from wisdom teeth removal in the office setting to complex procedures like corrective jaw surgery and facial trauma reconstruction.”
The team manages a diverse caseload, from outpatient dental extractions to hospital-based interventions for facial trauma. As a Level I trauma center, ChristianaCare relies on the oral and maxillofacial surgery team to address facial injuries year-round. Their role has only grown in complexity with the addition of surgeons trained in oncology and reconstructive techniques, including microvascular free tissue transfer.
One of the department’s most distinctive offerings is total joint replacement of the temporomandibular joint (TMJ), a highly specialized procedure offered by only a few centers.
“Much like you would get a hip or knee replacement, we do the same thing for the TMJ,” Dr. Meara said.
Currently, there are only two FDA-approved prostheses for the procedure: A stock option and a custom-designed joint. The ChristianaCare team primarily uses the custom version, which is engineered to the patient’s unique anatomy.
“What we’re custom designing is patient-specific for their total joint replacement,” Dr. Meara said. “This is ideal for patients who have failed nonsurgical and often other surgical options.”
The team is also using computer-generated, virtual surgical plans in order to better illustrate and explain complicated procedures to patients.
Beyond surgical innovation, the department is playing a growing role in managing oral cancer, a condition with increasing incidence, due to human papillomavirus-related cases in younger populations, among other factors.
“There are approximately 50,000 cases in the U.S. each year, but oral cancer doesn’t get the same attention as other cancers,” Dr. Meara noted. “We’re working closely with the Helen F. Graham Cancer Center and our ENT [ear, nose and throat] colleagues to provide multidisciplinary, comprehensive care.”
This collaboration spans not only tumor resection but also complex reconstructive challenges, he added.
“It’s not just about removing the cancer,” Dr. Meara said. “It’s about how we rebuild the face and restore function afterward. This is a really important discussion for patients in Delaware.”
“ChristianaCare’s head and neck team, comprised of ENT, plastic surgery, and OMFS is able to offer head and neck cancer surgery and reconstruction, including free flaps for large facial defects,” Dr. Meara said. “You’d have to go to Philadelphia or Baltimore to find similar work being done at this scale in the region.”
This summer, a new fellowship-trained surgeon will join the team, further bolstering ChristianaCare’s capabilities in maxillofacial oncology.
As the field of oral and maxillofacial surgery continues to evolve, ChristianaCare's team is committed to remaining at the forefront by integrating innovation, academic rigor and compassionate care. With an eye on expanding access and refining surgical techniques, the OMFS team is shaping a model for regional excellence in a truly hybrid specialty.
For patients with end-stage kidney disease, dialysis represents survival but not necessarily life. Kidney transplantation of any type offers a dramatically different outcome, significantly extending life expectancy and improving the quality of that life. The best outcomes of all are seen when a kidney is provided by a living donor. At ChristianaCare, the Living Donor Kidney Transplant Program gives people the opportunity to gift this lifesaving intervention to a patient in need.
“On hemodialysis, patients are typically sitting in a hemodialysis center three days a week for probably four hours each visit. They have two large needles placed in their arm, and they’re stuck there with this machine that cleans their blood. Without that dialysis, their life expectancy would be measured in days to weeks,” explained Jason Rolls, M.D., Surgical Director of the Kidney Transplant Program at ChristianaCare. “Some patients choose peritoneal dialysis, rather than hemodialysis. They have a tube placed in their abdomen, and they dialyze by passing large amounts of fluid through it, letting it sit inside them for hours before it is drained out. Either method of dialysis is a horrible way to live, for most people.”
“Statistically speaking, if you put a hundred adults, comprising a range of ages and medical conditions, on dialysis today, half of them will no longer be with us in just under four to four and a quarter years,” he added. “Transplanting people at any age from childhood into their 60s statistically more than doubles life expectancy. Even well-selected patients in their late 70s can enjoy twice as many remaining years.”
Most kidney donations come from deceased organ donors. While these kidneys provide excellent outcomes, waitlists can be long, and patients may get sicker while they wait for their opportunity for transplantation. Living donor recipients typically receive their transplant within months rather than years.
Living donor kidneys, coming from carefully screened healthy individuals during scheduled procedures, statistically last twice as long as deceased donor kidneys. This extended graft survival means that recipients receiving proper medical care can expect decades of function from a living donor kidney.
Kidney donation is a significant personal commitment, but its impact on a recipient cannot be overstated. ChristianaCare’s program addresses common barriers to living donation to ensure that almost every willing and able donor candidate will go on toto help a patient in need. Even when blood type or tissue compatibility issues exist, the program can arrange for paired kidney exchanges with other transplant centers by virtue of its participation in the National Kidney Registry, allowing these barriers to be overcome.
“Being part of the largest and most productive paired exchange organization in the country means that things like ABO blood group compatibility or immunologic incompatibility between an otherwise willing and medically appropriate donor and recipient pair should never be a barrier for us,” Dr. Rolls explained.
As people consider giving a gift of one of their kidneys to another, it is important for them to know the following:
- Statistically, someone who has donated a kidney ends up living longer than the general population. (They do not live longer because they donated their kidney, but because they are healthier than the general population to begin with.)
- Statistically, someone who has donated a kidney is not at increased risk for developing end-stage renal disease than does the general population.
- From the moment the potential donor candidate picks up the phone for the first time to call their transplant center and inquire about the process to the moment they are put to sleep for the donation surgery, they can change their mind and opt out. They maintain control over their own destiny as far as the living organ donation process is concerned, and their decision is final.
- Undergoing evaluation to be a living donor is likely to be the most diagnostic testing these patients have ever received (at no cost). Imaging, blood testing, heart and kidney function testing, evaluations by physicians, and other assessments are all free to the donor candidate, even if they later opt out.
- Medical information revealed during the living donor candidate’s evaluation process remains private, between the candidate, their physicians and their medical chart. Nothing concerning their medical information can be revealed to anyone else, including their intended recipient, without their express permission.
ChristianaCare’s kidney transplant program has experienced significant growth, increasing from 15 transplants in 2020 to 54 in fiscal year 2025. Despite the program’s growth ChristianaCare’s Transplant Team has maintained its commitment to the personalized care that it has always embraced.
“Every patient is an individual, with their own journey. We are here to ensure that journey is as successful as possible for them,” Dr. Rolls said.
Looking ahead, ChristianaCare continues to embrace innovations that expand transplant opportunities.
“Surgeons like ours are working harder and more thoughtfully to use deceased-donor organ opportunities that we are offered, many of which we would not have seriously considered five to 10 years ago, and we have found that they do quite well. Our community continually pushes this envelope in the interest of allowing our patients to live longer, healthier lives, filled with hope,” Dr. Rolls said. “However, living donation remains the best possible current routinely available option for anybody with end-stage renal disease. People willing to give someone else a kidney remain all too rare and precious. We look forward to further efforts at increasing public awareness and to the day when they are less rare.”
Adults who have moderate to severe obstructive sleep apnea (OSA) may benefit from a surgical option known as maxillomandibular advancement (MMA). ChristianaCare is currently one of the few health systems in the region performing this surgery
The American Academy of Sleep Medicine estimates that at least 25 million people in the United States have OSA. The condition occurs when muscles and soft tissue in a person’s throat repeatedly relax and collapse during sleep, blocking their airway and causing recurrent waking to restore breathing, which can seriously disrupt sleep and lead to reduced blood oxygen levels, according to Daniel J. Meara, MD, DMD, FACS, the chair of ChristianaCare’s Department of Oral and Maxillofacial Surgery and Hospital Dentistry.
Some of the major risk factors for OSA include obesity, smoking, alcohol consumption, asthma and chronic nasal congestion.
Men are several times more likely to have OSA than premenopausal women; however, the prevalence among women increases following menopause, Dr. Meara said. While the condition may affect people at any stage of life, it’s most common in middle-aged and older adults.
Symptoms of OSA include loud snoring, difficulty sleeping, pauses in breathing while asleep, frequently waking to urinate, morning dry mouth, headaches, daytime sleepiness, impaired concentration and impotence. Left untreated, Dr. Meara warned that the condition can cause a host of health concerns.
“People with OSA are at higher risk for hypertension and cardiovascular disorders, such as irregular heartbeat, heart attack and stroke,” Dr. Meara said. “They’re also more likely to develop metabolic syndrome, diabetes, liver disease, cognitive impairment, depression and anxiety. Further, when OSA is poorly controlled, there is significant negative impact on quality of life. That’s why it’s so vitally important that they receive treatment.”
For adults, making lifestyle changes or using oral appliances may be sufficient for managing the condition in its mild form, but those with moderate to severe disease typically require continuous positive airway pressure (CPAP) therapy, which is the gold-standard for treatment. However, compliance with CPAP can be low, necessitating alternative treatments, primarily surgery. Surgical options include uvulopalatopharyngoplasty (UP3), hypoglossal nerve stimulation (HNS; which uses an implanted electronic device to open a patient’s airway during sleep) and maxillomandibular advancement jaw surgery, according to Dr. Meara.
However, when UP3 and HNS techniques either aren’t appropriate or have failed to resolve the problem, MMA has proved to be a strong alternative.
“The surgery is performed on patients in a hospital operating room under general anesthesia,” Dr. Meara said. “MMA involves making incisions in the upper and lower jaw bones and moving them forward. This opens the upper airway to enhance airflow and improve breathing during sleep. The procedure generally lasts several hours and requires a hospital stay.”
Possible postoperative side effects include pain, bleeding, swelling, nasal congestion, teeth bite changes, weight loss, and temporary numbness in the lips, mouth or face. There also is a minor risk for complications, including infection and damage to teeth.
In most cases, patients are able to return to their daily activities and work in approximately four to six weeks.
“Research has found that MMA is highly effective, with a high success rate,” Dr. Meara noted. “For patients, the biggest benefit is that the procedure is a more permanent solution to OSA, whereas many of the other treatments require the nightly wearing of sometimes uncomfortable equipment that have their own side effects.”
Patients seeking state-of-the-art eye care in Delaware can now receive virtually all types of ophthalmic surgery close to home, as ChristianaCare has added three new fellowship-trained physicians to the staff within the past two years.
Glaucoma specialist Tomilade Adepoju, MD, who completed her ophthalmology residency at Nassau University Medical Center, in East Meadow, N.Y., and her glaucoma fellowship at Boston University Eye Associates, came on board in September 2022. Medical retina and uveitis specialist Benjamin Christopher Chaon, MD, the medical director of the Wilmington Eye Clinic and an associate professor of ophthalmology at Temple University, in Philadelphia, joined the staff in the summer of 2023. And, most recently, ChristianaCare has recruited the first neuro-ophthalmologist in the state of Delaware, Muhammad Asad Fraz, MD, who completed his neurology residency at Henry Ford Hospital, in Detroit, and a fellowship in neuro-ophthalmology at the University of Pennsylvania, in Philadelphia.
“Between the three of us, we are able to cover just about every area of ophthalmology, which means that we no longer have to refer patients with very complex eye conditions to practices in Philadelphia or Baltimore,” Dr. Adepoju said. “Our program is also affiliated with the Temple University ophthalmology residency, an exceptional training program, so we have residents who operate with us and learn from us in the clinic and operating room.”
As the population continues to age, the demand for cataract surgery is growing dramatically.
“We perform the simplest to the most complex surgeries,” she said. “Because we offer these procedures in the hospital setting, where we can manage patients holistically in collaboration with our colleagues in rheumatology, endocrinology and critical care, we are particularly well suited to care for the most challenging and difficult cases, such as people with long-standing diabetes and many other comorbidities. The majority of our patients are already somehow being cared for within the ChristianaCare system, so having the whole care team under the same umbrella is very helpful.”
Surgeries are performed at ChristianaCare’s Wilmington Hospital, which is also the primary location for the ophthalmology practice. Here, patients have access to laser procedures, minimally invasive surgeries, and traditional surgical options depending on their clinical situation.
“In this facility, we have a new Heidelberg Spectralis optical coherence tomography machine, which provides noninvasive imaging of the retina for the diagnosis of retinal disease and allows us to assess the optic nerve for patients with glaucoma,” Dr. Adepoju noted. “We also have two lasers for the treatment of glaucoma that may not yet be at the point of needing traditional incisional surgery, as well as a micropulse photocoagulation laser to treat more severe glaucoma in the OR setting. All of our equipment is state of the art.”
Within the next one to two years, the group also hopes to expand to a second location offering medical and surgical ophthalmic services at Christiana Hospital in Newark. Demand is high: Both Drs. Adepoju and Chaon are booked into early 2025 and Dr. Fraz through March 2025. However, the practice has dramatically increased the number of patients it is able to see, conducting between 300 and 400 diabetic screenings per month and performing between 10 and 14 surgeries monthly for each surgeon. The team works closely with referring providers to ensure that patients who need urgent ophthalmic care can be evaluated at ChristianaCare in a timely fashion.
“We also plan to expand and add one more specialist to the ophthalmology team within the coming year,” Dr. Adepoju said. “We are growing very quickly because there is such a need in this community for ophthalmic surgical care.”
When patients undergo imaging studies such as MRIs, CT scans and ultrasounds to screen for a variety of cancerous or noncancerous conditions, sometimes the scan reveals an unexpected finding: a nodule on the thyroid.
“Someone may have a traumatic injury and get a CT scan of their entire body, or they are experiencing neck pain or a muscle sprain or an issue with their cervical spine, and they get an MRI,” explained Leon Kushnir, MD, FACS, a fellowship-trained endocrine surgeon who joined the staff at ChristianaCare’s Helen F. Graham Cancer Center & Research Institute in the summer of 2024 after several years as the program director of the general surgery residency program at Inspira Health Network in southern New Jersey. He joined an experienced team that includes Arvind Sabesan, MD, FACS, a surgical oncologist with a special interest in endocrine surgery, and Alison Segal, a physician assistant with more than 25 years of surgical expertise.
“During that imaging, an incidental thyroid nodule is seen, which suddenly becomes a significant concern for the patient,” Dr. Kushnir continued. “They don’t really know how to react. Could it be cancerous?”
Many patients experience a lot of anxiety after they are told about this finding and want to be seen by an expert as soon as possible. Although the vast majority (up to 90%) of thyroid nodules are benign, they still require proper management—and patient education and consultation.
With Dr. Kushnir’s assistance, ChristianaCare has launched a new clinical pathway for the management of thyroid nodules. This process removes the burden of these findings off of the referring physician and immediately puts the case in the hands of an expert.
“When an incidental thyroid nodule is identified on imaging, it is flagged on the radiology report and the ordering physician is immediately given the information to refer the patient to myself or my partner, Dr. Sabesan,” Dr. Kushnir explained. “We will take care of everything from there.”
Within the past 10 years, genetic analysis has significantly improved the ability of surgeons, like Dr. Kushnir, and the pathologists he works with to accurately diagnose these nodules.
“When I first started my training, biopsy results were not very specific. We often performed extensive diagnostic surgeries on nodules that turned out to be benign,” he said. “Today, it’s relatively unusual for us to be doing a surgery when we don’t know definitively whether or not it is cancer.”
Dr. Kushnir envisions the thyroid nodule clinical pathway as a seamless process for the patient and the referring provider.
“Apple is very successful and famous because they make it very easy to use their products,” he noted. “We need to also make it very easy for our colleagues and patients to get expert care in a timely and easy fashion. One or two clicks will enable our referring providers to contact us, and we will get the patient in our door for a workup and in-office biopsy as soon as possible.”
Most of the time, incidental thyroid nodules turn out to be benign; Dr. Kushnir estimated that they are cancerous only between 5% and 10% of the time. However, time is still of the essence with these findings; “a lump on the thyroid” often still represents an emotional emergency to the patient.
“In my experience, whenever a patient sees that sort of incidental finding, they get very scared,” Dr. Kushnir said. “That’s especially acute when somebody has a personal or family history of cancer.”
Unfortunately, in the past, it could often take several months between identifying an incidental thyroid nodule on a scan and finally ruling cancer in or out.
“We’re going to change that,” Dr. Kushnir noted. “We want to make that transition from identifying a nodule, to counseling and biopsy, to having an answer as easy and quick as possible. Our goal is to have the patient seen in our office within one to two weeks after the initial diagnosis. At this visit, they will have a full consultation with a biopsy of the nodule if necessary, and results available the following week.”
ChristianaCare’s Center for Breast Reconstruction is the only such program in Delaware offering microsurgery fellowship−trained plastic surgeons. This enables the program, which has three microsurgery-trained surgeons—two of whom are women—to offer the full range of breast reconstruction modalities, including flap reconstructive surgeries in which microsurgeons use a patient’s own body tissue to reconstruct the breast. Occasionally, patients request an all-female team, and ChristianaCare is able to provide that.
In flap surgery, the most common area where surgeons find tissue to use is the lower abdomen. If surgeons can’t use abdominal tissue, perhaps because the woman is too thin or has had surgery on the abdomen before, they may be able to use tissue from the lower back, buttock or upper thigh. Using a person’s own tissue to reconstruct a breast has several benefits. First, it allows for a more natural look.
“The biggest advantage is that the reconstructed breast is made up of your own body tissue and replaces like for like,” said Stephanie Caterson, MD, the director of the Center for Breast Reconstruction at ChristianaCare. “With flap reconstruction after a mastectomy, the breast is replaced with skin and fat from the lower abdomen, which feels very natural for the patient. It also ‘ages’ much like a natural breast. If a patient gains or loses weight, the flap tissue fluctuates with the body over time, resulting in long-lasting symmetry.”
The second benefit of flap surgery is that it doesn’t use implants that require a lifetime of annual visits for imaging and assessment.
“Implant reconstruction is a great option for many people, but we need to remember that they are manmade products that will undergo normal wear and tear,” Dr. Caterson said. “If the outer lining of an implant breaks, it should be replaced. We recommend annual clinic visits to monitor the implants, and after five years, we start performing implant imaging to ensure the implant is intact. With implants, there is the lifetime risk of potentially having multiple surgical interventions. There is not a lot of maintenance surgery that goes with flap surgeries.”
Third, flap surgery is a better option for patients who have undergone, or are going to undergo, radiation for their breast cancer treatment.
“Implants and radiation basically don’t get along very well,” Dr. Caterson noted. “With radiation, sometimes scar tissue can build up around the implant, or the skin around the implant can really tighten up and change the shape, look and feel of the implant. We often recommend flap reconstruction after radiation to bring healthy tissue into the radiated field.”
Dr. Caterson pointed out that ChristianaCare offers the full range of breast reconstruction options, from implant reconstruction all the way through the complex tissue reconstructions. She said flap surgery isn’t for everyone, as it involves longer procedure and recovery times than implant surgery.
The most common type of flap surgery is the deep inferior epigastric perforator (DIEP) flap, which uses the lower abdominal skin and fat to reconstruct the breast. DIEP flap surgeries can take between four to eight hours for one breast or eight to 12 hours for two breasts. A patient must be otherwise healthy to be considered a good candidate for this long procedure.
“Basic implant reconstruction may be one or two additional hours if you are doing it at the same time as the mastectomy,” Dr. Caterson said. While an implant surgery involves one night in the hospital and then usually a three-week recovery, DIEP involves three to four days in the hospital and six to eight weeks recovery time, she added.
“What sets our group apart is that each of our fellowship-trained microsurgeons offers the full range of breast reconstruction options, creating personalized surgical plans tailored to each patient’s medical needs and personal preferences.” Dr. Caterson noted.
Another unique part of the breast reconstruction care practice at ChristianaCare is the team approach with surgeons, physician assistants, schedulers, office staff and medical assistants all working together cohesively.
“I can’t tell you how proud I feel when I’m sitting in my office and I overhear a patient stop at our medical assistant’s desk on the way out to thank them for being so kind and supportive, or helping them with their drain, or whatever it might be,” Dr. Caterson recounted. “A breast cancer diagnosis is often the most challenging thing a woman has gone through in their life, and we would like our office to be a support system for them. We try to be the silver lining of what they have gone through
Robotic technology allows colorectal surgeons at ChristianaCare to perform complex abdominal surgeries to treat patients and save lives. Indeed, the techniques enabled by robotics can improve patient outcomes and reduce costs of care.
Caitlyn M. Costanzo, MD, is a distinguished general and colorectal surgeon at ChristianaCare. She performs a wide variety of surgical procedures for the treatment of benign and malignant colorectal pathology. This includes segmental small and large bowel resections, low anterior resections (LAR), abdominoperineal resections, and complex reconstructions to restore bowel continuity. In the past, Dr. Costanzo primarily used laparoscopy for her procedures. Now, she has successfully incorporated the da Vinci Xi (Intuitive Surgical) surgical technology into her surgical practice.
The da Vinci Xi is a robotic surgical system that includes a patient cart that consists of four surgical arms and a surgeon console, where Dr. Costanzo sits and controls the robotic arms. The enhanced technology enables surgeons to visualize human anatomy in high-definition 3D. The surgical arms have multiple degrees of freedom and have built-in tremor-filtration technology. With the assistance of Firefly fluorescence imaging, Dr. Costanzo can identify important anatomy and ensure that the blood supply to the intestine is adequate for healing.
“Robotic surgical technology can improve patient outcomes by reducing intestinal manipulation,” she explained. “The entire surgery can be performed within the abdominal cavity, which allows patients to recover bowel function sooner.”
What Dr. Costanzo is referring to is an intracorporeal anastomosis, or ICA. Once a segment of intestine is removed, the restoration of bowel continuity is performed in the abdomen, so that there is no exposure of bowel to the outside environment. The reduction of external intestinal manipulation allows patients to have a quicker return of bowel function and thereby a shorter length of stay. Dr. Costanzo’s robotic surgery patients leave, on average, 1.5 days sooner than laparoscopic patients.
The robotic platform is especially helpful in certain patient populations. When the human anatomy makes it difficult to see or feel, the robotic technology enables surgeons to work in confined spaces, for example deep in the pelvis. Additionally, the ability to restore intestinal continuity while inside the abdomen means that the challenges of being able to deliver the intestine outside of the body are obsolete.
“Surgical technology is always advancing, yet I believe that robotics has proven to be the biggest advancement during my generation of surgery,” said Dr. Costanzo.
She is excited to be able to offer this modality to her patients.
With all the hype surrounding the new weight-loss medications, glucagon-like peptide-1 receptor agonists (GLP-1 RAs), clinicians may be getting questions from patients about treating morbid obesity via pharmacotherapy versus bariatric surgery. So, what can—and should—clinicians tell these patients?
“Medications are for short-term weight loss, are more expensive, have less of an effect and they provide less sustainability,” said Mingwei Ni, MD, a bariatric surgeon at ChristianaCare. “Bariatric surgery is obviously more invasive, but it is more effective in the treatment of morbid obesity and its associated diseases. Surgery works much faster than medication and will maintain weight loss for a lifetime. Patients who undergo bariatric surgery will lose 60% to 70% of their excess body weight versus 20% to 30% with medication. That is a huge difference.”
Roughly one-third of Americans are obese, and more than half of these people are considered morbidly obese (body mass index, ≥40 kg/m2). Morbid obesity is one of the main causes of many chronic and life-threatening diseases, including hypertension, type 2 diabetes, stroke, coronary artery disease, heart failure, kidney failure and peripheral vascular disease. Morbid obesity is also a very strong risk factor for numerous types of cancer, including breast and colon cancer.
Weight-loss medications have been on the market for 30 years, with many of the older drugs working by, for example, suppressing the absorption of fat or by increasing metabolism. The GLP-1 RAs, currently injectable medications, work by making the stomach wall move less, thus keeping food in the stomach longer. The result is that people feel full very quickly and are less hungry.
The two most common options for bariatric surgery are sleeve gastrectomy and gastric bypass. While bariatric surgery can treat the medical comorbidities that are associated with morbid obesity, the GLP-1 RAs are only able to treat diabetes—and not as well as bariatric surgery.
“Weight-loss surgery will help you lose weight in order to treat comorbidities such as diabetes, hypertension and sleep apnea, and will prevent heart attack and stroke,” Dr. Ni said. “The newer weight-loss medications don’t really treat these medical comorbidities, and the medications can cause GI symptoms that people can’t tolerate, such as stomach pain, nausea, vomiting, diarrhea and heartburn.”
Surgery also has a much higher chance of bringing patients’ BMI back to a healthy level. Of note, the weight loss is a more sustainable option compared with weight-loss medications. For example, with the GLP-1 RAs, when patients stop using them, they usually gain the weight back.
“Bariatric surgery will hopefully last a lifetime, especially if the patient is willing to change their lifestyle and work with a dietitian,” Dr. Ni said.
The new weight-loss medications are also very expensive at roughly $1,000 per month per patient, he added.
“The cost of surgery is much lower and insurance covers it,” Dr. Ni said. “The copay out of pocket depends on insurance, but Medicaid and Medicare almost cover 100%.”
That said, sometimes both bariatric surgery and weight-loss medications are used concomitantly.
“Weight-loss treatment can be a combination of the medication, surgery and lifestyle changes such as diet and exercise,” Dr. Ni noted. “It’s a really multidisciplinary approach to treat this disease.”
At ChristianaCare, a team approach is used to treat a patient with morbid obesity.
“It’s very important to work with a well-trained experienced team of dietitians, psychologists, a physician who will optimize the patient for surgery, bariatric surgeons, a nurse practitioner who can follow the patient long term and a support group for patients to attend before and after surgery,” Dr. Ni explained.
For example, ChristianaCare offers free online educational seminars for patients given by two bariatric surgeons. They also offer a 174-page healthy recipe book on the ChristianaCare bariatric website, which is free for download.
“In general, weight-loss surgery is as safe as gallbladder surgery or knee replacement surgery. It’s a small incision to do the surgery,” Dr. Ni said. “We offer outpatient sleeve gastrectomy for patients with suitable indications.”
Dr. Ni added that all patients undergoing bariatric surgery go home without the need for narcotics. “Pain is usually controlled by non-narcotic medications such as [acetaminophen] and a muscle relaxant,” he said. “Bariatric surgery is a very good and a very safe option.”
Bariatric surgeons at ChristianaCare are using weight-loss procedures as a tool for patients with obesity to foster improved health metrics across a number of disease states.
Patients undergoing Roux-en-Y gastric bypass and sleeve gastrectomy have not only lost weight but have also seen positive improvements in comorbid type 2 diabetes, hypertension, and cardiovascular and kidney disease, as well as reduced levels of low-density lipoprotein (“bad cholesterol”) and hemoglobin A1c. Many of these patients have struggled maintaining a healthy weight despite other interventions such as exercise programs, dietary changes and even medications, according to Elizabeth McCarthy, MD, a minimally invasive bariatric surgeon at ChristianaCare.
“For a lot of patients, bariatric surgery is the last stop in their weight-loss journey,” Dr. McCarthy said. “They have been living with obesity for some time and are dealing with a number of health complications as a result. Some have even been told they will die unless they lose weight and have the surgery. Our goal at ChristianaCare is to guide these patients and their families through surgery, and we provide them with support before, during and after their procedures to help them get the best results.”
Because of type 2 diabetes, cardiovascular disease, kidney disease and hypertension, among other potential health problems, many patients undergoing bariatric procedures—most of which involve sleeve gastrectomy at ChristianaCare—are on multiple medications before surgery. However, after surgery, most patients can expect to take medications at lower doses or come off them altogether, according to Dr. McCarthy.
However, management of these patients doesn’t stop immediately after surgery. In fact, patients are monitored postoperatively for an indefinite period to ensure they are maintaining a healthy weight and still doing well with any comorbid conditions, she said.
“If they are struggling with weight, even postoperatively, we provide them with the education and resources they need to get back on track,” she added.
This education is actually a continuation of the patient instruction that begins preoperatively. Before surgery, patients typically meet with a nutritionist to review their diet and a psychiatrist to assess for underlying disordered eating or mental health conditions that may contribute to weight gain or hinder weight loss.
In addition, ChristianaCare has developed an online seminar that patients are encouraged to view before their initial surgical consultation. It reviews what to expect in the lead-up to surgery, during the procedure and after it. Primary care physicians and practitioners should encourage patients who are interested to sign up and learn more about bariatric surgery, Dr. McCarthy said.
On top of that, bariatric surgery patients at ChristianaCare are required to take several virtual classes, via Microsoft Teams, delivered by the Weight Management team. These classes advise patients on diet and exercise and, in general, “how to stay committed and engaged in their health journey” after surgery, Dr. McCarthy explained. “There’s a lot of work that’s involved getting to surgery, and it can take up to a year.”
That said, the goal is not to make the process more difficult; rather, it’s designed to ensure success. Currently, bariatric surgery is recommended for adults with a body mass index more than 35 kg/m2 and a medical comorbidity such as type 2 diabetes, hypertension and sleep apnea, as well for those with a BMI greater than 40 kg/m2, as they are at increased risk for these and other comorbidities, including infertility and polycystic ovary syndrome. However, less than 1% of patients who meet the criteria for surgery nationally ultimately are referred for these procedures.
“A lot of that is due to the stigma surrounding obesity,” Dr. McCarthy explained. “That’s why it’s so important for us to create an environment where patients feel supported.”
Some of that support is provided by the patients themselves. The bariatric surgery team at ChristianaCare oversees a monthly online support group led by patients who have had the procedure within the system and includes topics from the team’s dietitians, surgeons and other providers directly involved in the bariatric patient’s care.
“Patients share their experiences and encourage each other to maintain a healthy lifestyle and get the most from their surgery,” Dr. McCarthy said. “Surgery is a great tool to get you where you want to go, but it’s just that: a tool. Patients will need to keep working to be successful, and being successful requires support. That’s why we strive to have an excellent supportive practice with a multidisciplinary team that works with all of our patients preoperatively and postoperatively. That separates ChristianaCare from a lot of surgical practices.”
When a patient presents with complicated diverticulitis—with perforation, abscess, obstruction and/or fistula—to ChristianaCare, admission to the hospital is usually required.
Indeed, if the patient has peritonitis, surgical removal of a portion of the colon is required. Traditionally, this would entail removal of the sigmoid colon and creation of a colostomy. More recently, however, research has shown that it is safe and effective to remove the sigmoid colon and divert stool via an ileostomy, according to David C. Palange, DO, a colon and rectal surgeon at ChristianaCare’s Helen F. Graham Cancer Center and Research Institute. At ChristianaCare, this procedure is performed using state-of-the-art tools and approaches.
“If you become my patient, particularly for elective procedures, you’re getting a robotic or laparoscopic surgery with all incisions the size of my thumbnail,” Dr. Palange said. “Through minimally invasive techniques for robotic-assisted or laparoscopic surgery, you definitely decrease the chances of wound infection and pain.”
In fact, with the use of the robot, “the surgeon can suture and staple and perform other tasks” more quickly and accurately, reducing the risk for postoperative infection, time under anesthesia and other potential complications, he added.
A colostomy reversal remains a challenging procedure due to residual scar tissue. In contrast, ileostomy reversal is relatively easy for the surgeon to perform. As a result, with ileostomy a patient can anticipate a fuller recovery, restoring normal bowel movements, according to Dr. Palange.
Patients undergoing colostomy have about a 50% chance for reversal, but the percentage with ileostomy is much higher, he said.
Recovery times from surgery for complicated diverticulitis vary, Dr. Palange added. If a minimally invasive surgery is performed using enhanced recovery after surgery protocols, a patient typically stays in the hospital two to five days, with recovery expected to take two weeks and complete healing taking place within six weeks. With open procedures, hospital stays and recovery and healing times are much longer, Dr. Palange said.
Generally, about one in four patients with diverticulitis develop complicated disease. For the far more common uncomplicated, non-severe form of the condition, which involves localized inflammation of the diverticulum, a more conservative treatment approach is used.
Traditionally, uncomplicated diverticulitis has been managed with antibiotics and a liquid diet, and most patients recover at home without hospitalization. However, at ChristianaCare, Dr. Palange and his colleagues adhere to updated guidelines from the American Gastroenterological Association, which recommend “selective, rather than routine, antibiotic use in immunocompetent patients with mild disease.”
While antibiotics have long been the first-line therapy for acute uncomplicated diverticulitis, recent evidence suggests there is no benefit from their use in immunocompetent patients with mild acute uncomplicated diverticulitis, according to Dr. Palange.
“Historically, the use of antibiotics for acute cases has been in response to what was believed to be an immediate infection, but it is now understood that it’s the inflammation and not the infection that causes the symptoms,” he said. “This newer approach of selective use of antibiotics has not yet been widely adopted, but we’re using it here to prevent overuse of antibiotics, which can later lead to resistance and unnecessary side effects.”
Dr. Palange added: “Colonic diverticulitis remains a painful, unpredictable gastrointestinal disease that can lead to serious complications, chronic symptoms and poor quality of life. At ChristianaCare, we strive to use the latest, evidence-based approaches to give our diverticulitis patients the best possible outcomes.”
Evolving screening techniques, coupled with minimallyinvasive surgical solutions, are allowing physicians at ChristianaCare to look beyond gallstones in caring for patients with abdominal pain.
“We used to always think there was only one issue with the gallbladder—gallstones,” said Michael B. Goldberg MD, a minimally invasive surgeon practicing at ChristianaCare. “Now we know that it’s not actually only gallstones that give people gallbladder symptoms and upper right quadrant pain. There is much more to it.”
Patients experiencing this type of pain, which is often quite debilitating, may have biliary dyskinesia, a condition in which the gallbladder is not squeezing as hard or as fast as it should. Biliary dyskinesia can result in insufficient amounts of bile being ejected from the gallbladder into the small intestine.
Conversely, some patients may also have biliary hyperkinesia, when the gallbladder squeezes too fast and too hard, causing recurring biliary colic.
Both conditions can cause significant pain and discomfort. However, when testing indicates no presence of gallstones, patients’ pain would often go untreated.
“People who were suffering from right upper-quadrant abdominal pain and the inability to tolerate meals would get an ultrasound and it would look normal—with no gallstones—and we thought that was the end of the story,” Dr. Goldberg said.
Now, hepatobiliary iminodiacetic acid (HIDA) scans allow for far more detailed review of gallbladder function, enabling specialists to more properly identify the cause of their patients’ symptoms.
“The HIDA scan can show us exactly how the gallbladder is functioning, and allows for more investigation in order to help our patients who are experiencing gallbladder symptoms without gallstones,” Dr. Goldberg said.
If the gallbladder is determined to be functioning incorrectly and needs to be surgically removed, current techniques allow for far easier procedures with greatly reduced recovery times.
“We use the latest minimally invasive techniques including laparoscopic and robotic surgery with smaller incisions,” Dr. Goldberg said. “It used to be that people needed to stay in the hospital when they had gallbladder surgery. Now it is done on an outpatient basis.”
Most people are able to manage the discomfort of gastroesophageal reflux disease (GERD) with lifestyle changes and medications. However, patients who have failed medical management or who don’t want to be on proton pump inhibitors, due to potential side effects, are candidates for surgery, according to Anthony R. Tascone, MD, a bariatric and foregut surgeon at ChristianaCare.
Other patients should be considered candidates for a surgical intervention are those who have Barrett’s esophagus, esophagitis or stricture from changes in their esophagus from reflux, he said. For all surgery patients, Dr. Tascone and his colleagues are using state-of-the-art procedures to achieve optimal outcomes in GERD.
For decades, fundoplication has been the gold standard for GERD surgery. During the procedure, the surgeon takes the top part of the stomach and wraps it around the bottom of the esophagus, with the goal, essentially, of bolstering the lower esophageal sphincter (LES). The procedure can entail a partial or total (Nissen) wrap, depending on the severity of esophageal motility.
Today, these procedures are minimally invasive and many surgeons at ChristianaCare are performing GERD surgeries robotically. Following surgery, most patients see improvement in their symptoms and can either be taken off medications completely or continue them at lower doses. More than four in five patients undergoing these procedures will see complete resolution of symptoms, with no need for medication.
“There are pluses and minuses to each of these approaches while the surgical outcomes for both are excellent,” Dr. Tascone said. “An important benefit of fundoplication is that the patient’s native tissue is used.”
Another GERD procedure performed at ChristianaCare involves implantation of the LINX reflux management system (J&J Med Tech), a novel device composed of a ring of magnets designed to strengthen the LES. Following surgical insertion, the LINX device is in the “closed position most of the time” to keep acid in the stomach, according to Dr. Tascone.
“The LINX has the ability to open and close so that food and drink can pass through it and patients can burp or vomit, as needed, when air forms in the stomach,” he said. “That is harder to do following fundoplication.”
In general, outcomes following LINX implantation are similar to those for fundoplication, which research leads to improved symptom control and quality of life in 90% of patients.1 Still, a downside of LINX is that up to 40% of patients develop dysphasia during the few months following the procedure.2
Another recent addition to the surgical armamentarium for GERD at ChristianaCare is gastric bypass, particularly for patients with elevated body mass index. In addition to treating GERD, gastric bypass helps treat common comorbidities, including hypertension, type 2 diabetes, obstructive sleep apnea, and hyperlipidemia, by fostering weight loss.
“So, patients will get more bang for their buck when undergoing gastric bypass surgery,” Dr. Tascone said. “The outcomes for all of these procedures are very similar, though recovery is slightly different for each option. Laparoscopic surgery has a quicker recovery time and less pain than open surgery. The primary care doctor and the surgeon can work together to help decide which is best for the patient.”
References
- John M, Irvine T, Thompson SK, et al. Antireflux surgery in patients with gastroesophageal reflux but a negative 24-hour pH study—late outcomes. J Gastrointest Surg. 2024:S1091-255X(24)00449-9.
- Fadel MG, Tarazi M, Dave M, et al. Magnetic sphincter augmentation in the management of gastro-esophageal reflux disease: a systematic review and meta-analysis. Int J Surg. 2024 May 9.
At The Hernia Center at ChristianaCare, surgeons are using innovative technological approaches, paired with highly customized individual care plans, to provide cutting-edge treatment. The approach allows for low-risk procedures with faster recovery times, for patients with either minor or major surgical needs.
“Historically, patients have been a bit wary of hernia surgery for lots of different reasons,” said Peter M. Santoro, MD, the director of robotic surgery and medical director of The Hernia Center at ChristianaCare. “They may have heard from a friend or family member how painful it was, or how hard it was to recover from the procedure. Maybe they know people who had issues with mesh or other complications from their surgery.”
Much of this, according to Dr. Santoro, was due to the fact that hernia repair has often required open surgery necessitating large incisions. Too frequently, this meant that patients were faced with complicated procedures, long hospital stays and often painful, time-consuming recoveries.
However, over the past two decades, minimally invasive techniques have revolutionized many surgical specialties, hernia care included. As technology has rapidly advanced, developments in robotic surgery have allowed for previously unthinkable improvements in both surgical accuracy and patient recovery.
“From the smallest hernias to the most complex cases that require abdominal wall reconstruction, we’ve been able to move from big-incision operations to minimally invasive surgery,” Dr. Santoro said. "A huge part of that has been the advancement of robotic surgery, which has taken hernia treatment to a level that has never previously been seen, from a technical standpoint, as well as through patient satisfaction and recovery. It’s changed the way we take care of patients with hernias.”
The most recent advancement has been in the management of complex ventral hernias, which require abdominal wall reconstruction via transversus abdominis release (TAR) procedures.
“These TAR procedures traditionally could only be conducted as an open operation, and were reserved for the most complex ventral abdominal wall hernias,” Dr. Santoro said. “The postoperative course was typically very rocky, with significant complications on a fairly routine basis.”
Now, robotic abdominal wall reconstruction via the robotic TAR procedure has enabled surgeons to adopt novel techniques in order to vastly minimize the risks associated with these procedures.
“Robotic TAR has completely revolutionized the way we deal with complex abdominal wall hernias and abdominal wall reconstruction,” Dr. Santoro said. “It’s taken an operation that was associated with about a week-long hospital stay, with a high risk of perioperative complications, and reduced it to an overnight stay with very rare incidence of complications and a much easier recovery course for the patient.”
Currently, most patients undergoing hernia repair surgery—particularly when robotic techniques are used—can expect a same-day discharge from the hospital and a speedy return to normal activities.
“A minor subset of patients may require a one-night stay in the hospital, but the vast majority will be able to go home the same day,” Dr. Santoro said.
In addition, unlike with open procedures, postoperative pain following minimally invasive surgery can frequently be managed without the use of opioids or other narcotic medications. While heavy lifting and strenuous physical activity is typically limited for a four-week period, patients can expect to be up and about within hours of their procedure, a fact that strongly benefits the recovery process.
“I expect patients to be walking around, going up and down stairs, getting in and out of the car even the same day as the operation, and certainly by the next day,” Dr. Santoro said. “We don’t want patients to be sedentary after surgery.”
As the exact needs of patients depend upon multiple factors, Dr. Santoro and his colleagues put great effort into developing and communicating plans that are unique to each person.
“With hernia surgery, the surgical process is very patient-specific,” Dr. Santoro said. “It’s a highly tailored approach even compared with other types of medicine. Every patient that has a hernia is different, and we take a very individual approach for every patient. We provide comprehensive hernia care for the state of Delaware and the surrounding areas, and medical personnel should feel very confident that their patients will be well taken care of.”
For patients with uveitis, a rare inflammatory eye disease that can lead to blindness, advances in diagnosis and treatment are allowing for lessened therapeutic burden, with fewer side effects.
“Typically, we think of uveitis as having either infectious or noninfectious causes,” explained Benjamin C. Chaon, MD, medical director of the Wilmington Eye Clinic at ChristianaCare and an ophthalmologist who specializes in treating patients with ocular inflammatory and retinal diseases. “Uveitis can be associated with infections, such as syphilis, toxoplasmosis, or Lyme disease, or it can be noninfectious and associated with an underlying systemic autoimmune disease like sarcoidosis, rheumatoid arthritis, or inflammatory bowel disease. Or, it may not be associated with any underlying systemic disease and just impact the eye, such as Birdshot Chorioretinopathy.”
While the various types of uveitis share the basic feature of inflammation occurring in the vascular structures of the eye, the wide variety of causes can complicate diagnosis.
“The most important distinction we make in the initial diagnosis of uveitis is whether it’s infectious or noninfectious,” Dr. Chaon said. “Sometimes this can be difficult to determine, particularly if a patient develops uveitis following cataract surgery or another type of ocular surgery.”
In recent years, advancements in metagenomic deep-sequencing technology have helped to ease the diagnostic process. This technique allows ophthalmologists to take a small sample of fluid from the front part of the eye during a patient’s clinic visit and conduct testing to determine whether there is the presence of bacteria or fungus.
“This was not always possible in the past, as we often needed larger sample volumes to culture,” Dr. Chaon said. “This was difficult to do from the eye, as it is such a small space. This new technology allows us to more readily make the diagnosis of an infectious uveitic condition. That has been an exciting development in the field of uveitis in the last few years.”
Treatment, too, has advanced, moving beyond the use of corticosteroids. The advent of biologic therapies for the management of uveitis has allowed specialists to significantly decrease their reliance on steroids.
“It used to be that corticosteroids were the mainstay of uveitis treatment, but steroids have a lot of systemic side effects,” Dr. Chaon said. “Biologics are medications we use for patients with other rheumatologic conditions, such as adalimumab or infliximab, which target specific inflammatory molecules. Often these medications are helpful with getting control of the uveitis and allowing us to get patients off of—or to a lower dose of—steroids.”
Advances in regional steroid therapy have also allowed for more targeted treatment options with potentially fewer systemic side effects. For patients with vision-threatening complications of uveitis like macular edema, ophthalmologists historically relied on periocular steroid injections into the sub-Tenon’s space around the eye, with patients often requiring treatment every three to four months.
Recent data from the PeriOcular versus INTravitreal Corticosteroids for uveitic macular edema or “POINT” trial1 has demonstrated that intravitreal delivery of steroid medication directly into the vitreous cavity is superior to periocular steroid injections in the improvement and/or resolution of macular edema.1 Still, patients being treated with an intravitreal steroid medication, like the dexamethasone intravitreal implant (Ozurdex, Allergan), may need injections every few months, which can be quite burdensome, particularly for working-age individuals that uveitis disproportionately effects.
“That’s a lot of injections for patients, and every injection in the eye carries with it a small risk of infection,” Dr. Chaon said.
In contrast, the intravitreal steroid injection Yutiq (fluocinolone, Alimera Sciences) can provide up to 36 months of inflammation control in one dose. Another new medication called Xipere (triamcinolone, Bausch & Lomb) uses a novel drug delivery mechanism to allow the steroid to be injected into the suprachoroidal space—the area between the choroid and the sclera. Research has shown that this approach may result in more effective control of inflammation and a lower risk of increased intraocular pressure.
Although those with uveitis may require regular clinical visits to monitor their disease, reducing the frequency of injections can result in greatly increased patient satisfaction.
“In a lot of cases, uveitis tends to be a chronic disease, and patients do tend to need chronic treatment,” Dr. Chaon said. “So, treatment options that may lessen their treatment burden can be a big relief.”
Reference
- Thorne JE, Sugar EA, Holbrook JT, et al; Multicenter Uveitis Steroid Treatment Trial Research Group. Ophthalmology. 2019;126(2):283-295.
Neurosciences
People who experience seizures die at a higher rate than those who don’t, and 70% of seizure-related deaths result from asphyxiation caused by turning face down on the pillow during sleep. John Pollard, M.D., a neurologist and director of the Epilepsy Center at ChristianaCare, has developed a novel technology that can prevent these incidents: a headband that can alert another person in the same residence that a person with epilepsy is lying in this dangerous position.
“It’s been shown that if you can warn someone, then they can flip the patient over and save their life,” he said, adding that the headband works in much the same way that a cellphone’s accelerometer can tell the user the location of their phone. “In the case of this device, the accelerometer is in your headband and if the headband detects that your face is down while you are asleep, then it will sound an alarm. It first has a quiet alarm to warn the person themselves that they are face down and, if they can’t or don’t respond, then it will sound a louder alarm for a loved one or caregiver.”
The headband was made possible through a collaboration with ChristianaCare’s Health & Technology Innovation Center. To fully realize the potential of new technologies designed to impact health and improve patient care, ChristianaCare’s Health & Technology Innovation Center brings together clinicians and information technology experts to harness emerging technologies and develop unique solutions for delivering the best possible care.
Staffed with a team of award-winning software developers, designers and user experience analysts, the center collaborates with physicians, nurses and other healthcare professionals with new solutions to create a better experience of care and better health.
Dr. Pollard entered his idea into the Health & Technology Innovation Center’s Innovation Challenge, a biennial event that invites care providers to submit new ideas, apps or technology designed to improve patient care, enhance community connection and address relevant health challenges. Although Dr. Pollard did not win the challenge, the staff at the center believed the idea was worth developing.
“The idea was interesting enough that they developed a prototype and there is a patent pending,” Dr. Pollard said.
This innovative headband highlights how neurosciences continue to be at the forefront of advancing science and integrating cutting-edge technology to enhance patient safety, prevent seizure-related deaths, and ultimately provide better care.
Autism spectrum disorder (ASD) encompasses a range of limitations in reciprocal and communication developmental milestones, resulting in significant functional challenges throughout life. Although there is no consensus regarding the brain structures and mechanisms underpinning ASD, some researchers have focused on abnormalities that affect the mirror neurons and other cortical areas involved in social reciprocity, while others have proposed a more widespread alteration in neuronal organization resulting in abnormal white matter trajectories that lead to cortical over- or under-connectivity.
Mitra Assadi, M.D., and her team at ChristianaCare have focused their research on a target they define as “the social reciprocity network”—the mirror neurons in the inferior frontal gyrus (IFG) and inferior parietal lobule (IPL) of the brain, as well as the cortical areas involved in abstract social cognition, including the medial prefrontal cortex, temporal-parietal junction and posterior cingulate gyrus.
“We hypothesize that aberrant connectivity affecting the above neuronal circuitry, what we call ‘the social reciprocity network,’ contributes significantly to the core deficits in this condition,” explained Dr. Assadi, a pediatric neurologist the medical director for neuroscience education at ChristianaCare.

The research team is launching a study using quantitative electroencephalography (QEEG)-based coherence and spectral power analysis to measure the functional connectivity and neuronal dynamics involving the social reciprocity network in patients with ASD. The research protocol offers study participants noninvasive brain modulation, via repetitive transcranial magnetic stimulation (rTMS), which may mitigate the aberrant behaviors in ASD by altering neuronal dynamics and connectivity.
“Our overarching goal is to explore the neuronal connectivity and oscillatory patterns in the social reciprocity network and to elucidate the mechanism of modulating the above variables in improving social cognition,” said Dr. Assadi, who is also a professor of neurology at Thomas Jefferson University.
“Everyone has a tremor center of their brain,” Dr. Martello explained. “For patients with tremors it is not functioning correctly.”
The study, for which enrollment began in the fall of 2024, will involve 37 ASD patients ages 13 to 18 years. Participants will undergo 18 sessions (three times per week for six weeks) of rTMS or sham stimulation of the bilateral IPL/IFG in a prospective, single-blind study design. During phase I (three weeks), half of the subjects will receive rTMS and the other half will receive sham stimulation. During phase II (three weeks), all subjects will receive active rTMS.
The type of rTMS used in the study, known as intermittent theta burst stimulation (iTBS), is unique in inducing the production of brain-derived neurotrophic factor, leading to neuronal plasticity. Participants undergoing active treatment will receive 2,400 stimulations per session, divided equally between the bilateral IPL and IFG. The outcome measures include a neuropsychological battery (at baseline, phase 1 and 2, and three weeks after completing rTMS) and QEEG analysis (on the first and last active treatment sessions).
“The QEEG enables us to measure the coherence and spectral densities and determine if there is a reproducible pattern within the social reciprocity network in ASD,” Dr. Assadi said. “To measure the behavioral effects of rTMS/iTBS, we will use the Childhood Autism Rating Scale as well as the Social Responsiveness Scale. We expect to see an improvement in the behavior scores commensurate with enhanced social cognition, enhancement of the beta and gamma powers, and the connectivity within the social reciprocity network.”
Dr. Assadi explained that “this exploratory research builds upon our proof-of-concept testing of 11 children with ASD who received 10 sessions of rTMS targeting unilateral IPL.” The QEEG analysis performed in four subjects demonstrated an enhancement of beta and gamma powers post-rTMS in three cases, she added.
“We also demonstrated a modest improvement in social awareness,” Dr. Assadi said. “The rTMS/iTBS targeting of the bilateral social reciprocity network is a novel concept in ASD. Analyzing the correlation between the behavioral outcomes and the alterations in the neuronal connectivity and dynamics may provide a deeper understanding of the neuroanatomical substrate underpinning ASD, and inform the future clinical trials leading to effective and personalized treatment approaches.”
A patient diagnosed with multiple sclerosis (ChristianaCare’s pediatric neurology program provides comprehensive, continuity-focused care delivered by an experienced team of physicians. The program emphasizes collaboration with families and pediatricians to develop personalized treatment plans tailored to each patient’s needs, addressing both simple and complex neurological conditions by combining advanced diagnostics, cutting-edge treatments, and decades of expertise.
“We offer treatments for a range of neurological disorders, including common conditions such as headaches, Tourette’s syndrome, epilepsy, and attention-deficit disorder, as well as more complex issues like developmental delays and autism,” said ChristianaCare pediatric neurologist Mitra Assadi, M.D., medical director for neuroscience education. “We are able to define pediatric epilepsy syndromes based on findings from standard EEG recordings, ambulatory EEG, or long-term video EEG monitoring.”
According to the American Academy of Neurology guidelines, genetic testing is a crucial component of further assessing patients with developmental delays, explained Dr. Assadi, a professor of neurology at Thomas Jefferson University. At ChristianaCare, DNA samples are obtained via a simple oral swab provided during the initial consultation.
Genetic testing proves highly impactful, leading to precision cellular or molecular treatments in 15% to 20% of cases. Even when such treatments are not available, genetic testing offers significant benefits by concluding the diagnostic odyssey for patients and their families, Dr. Assadi noted.
“Many of these genetic syndromes involve multiple systems,” she explained. “Therefore, having a genetic diagnosis allows us to put the pieces of puzzle together and understand the big picture.”
Genetic testing can also provide useful information for future family planning and prognostication. Discovering a specific mutation in the patient will allow us to perform DNA testing on the unborn fetus and determine if the unborn child is going to be affected.
“Some parents may decide to abort a baby expected to have a poor prognosis,” Dr. Assadi noted. “We also provide targeted genetic testing for conditions such as muscular dystrophy or familial neuropathies. After establishing the diagnosis, we will refer these patients to specialized centers to receive cell/gene-based treatments. In addition to providing a great service, at ChristianaCare, we are committed to continuity of care. We are experienced and seasoned pediatric neurologists with 30 plus years of experience.”
In the skies over Delaware, ChristianaCare’s LifeNet air medical transport team is pairing cutting-edge aviation technology with critical care medicine to save precious moments in the race to treat patients who have experienced stroke and other trauma.
Navigating the complexities of patient transfer, prepping care teams and ensuring maximum efficiency from the time a stroke is first recognized can have a significant impact on preventing long-term disability and death. The LifeNet team is revolutionizing stroke and trauma care in Delaware by leveraging advanced aviation technology and streamlined processes to significantly reduce transfer times, ultimately improving patient outcomes and enhancing the chances of recovery.
“It’s estimated that roughly 1.9 million brain cells die every minute that a stroke goes untreated,” said John Roussis, MBA, NRP, FP-C, CMTE, the program director for pre-hospital services at ChristianaCare. “So, early recognition and activation is key. We work with ChristianaCare’s multidisciplinary teams to constantly try to improve our metrics, and to use high-performance efficiencies to get beds ready, notify clinicians, prep our laboratories and decrease time to treatment for these patients.”

On the ground, a custom “easy button” placed in referring community hospitals allows medical staff to immediately notify the pre-hospital team anytime a case may require a time-sensitive transfer. Pressing the button engages the pre-hospital communication center, which then places a helicopter or ambulance on standby. While that happens, information regarding the case flows into the center, helping to determine the correct response, either air or ground transport, and passing along critical information to hospital emergency departments.
“Even five years ago, we would have to wait for a physician to phone the center to request a transfer,” Roussis said. “Transport—the part of the process that often takes the longest to organize—would be activated four or five tick-marks into the response process. Now, we already have transport on the way well before the physician is done assessing the patient.”
The two LifeNet helicopters—one based at Christiana Hospital in Newark and the second at Delaware Coastal Airport in Georgetown—are staffed by flight teams accredited by the Commission on Accreditation of Medical Transport Systems and available 24/7 to provide emergency air transport for critically ill or injured adult, pediatric and neonatal patients.
Pilots of the aircraft are instrument flight rules—or IFR—rated, meaning they can fly while relying solely on reference instruments, allowing them to move efficiently through areas of differing airspace and safely navigate in adverse weather conditions. Additionally, the teams are cross-trained for both ground and air, meaning they are able to avoid significant delays in the event they are unable to fly.
As a result, in Delaware, stroke patients located in the farthest reaches of the state can often be transported to ChristianaCare more quickly than was previously possible; which is critical for patients needing urgent surgical intervention for treatment of their stroke. One hospital in southern Delaware experienced an 84-minute reduction in door-in-door-out times for these transfers, and similar rates have been seen among the other referring hospitals.
These time savings can have a significant impact on patient outcomes. Studies have shown that during stroke or transient ischemic attack, the brain ages by a rate of roughly 3.6 years per hour without treatment, and the effect of stroke on cognitive function is equivalent to 7.9 years of aging.1
“Every minute you save through this process gives somebody an increased chance of having less disability and a better chance of life,” Roussis said. “If you can save three or four minutes per step in this process, that can potentially mean the difference between long-term ventilator care and being able to return to work on Monday.” •
References
- Front Aging Neurosci. 2019;11:348.
“Neuro-ophthalmology overlaps with many fields of medicine—as the name suggests, it bridges the fields of neurology and ophthalmology,” said Muhammad Asad Fraz, M.D., a board-certified outpatient neurologist and fellowship-trained neuro-ophthalmologist at ChristianaCare’s Ophthalmology Wilmington Health Center. “It focuses on all ophthalmological disorders related to the central or peripheral nervous system.”
Patients referred for neuro-ophthalmology evaluations are often medically complex and have already seen multiple specialists. Typically, patients seen by Dr. Fraz are referred either from neurology, ophthalmology, neurosurgery or otorhinolaryngology (ENT).
By the time they meet with Dr. Fraz, they are seeking expert guidance for difficult-to-diagnose conditions. This includes patients with different issues including double vision, pseudotumor cerebri syndrome (also known as idiopathic intracranial hypertension), headaches, transient visual disturbances, brain tumors, stroke, optic nerve pathology, eye movement disorders and eyelid droop.
“Patients come to me with high expectations for the best possible care, and rightly so,” he explained. “Sometimes patients with brain or orbital tumors affecting vision benefit from neuro-ophthalmology assessments that may guide surgical decisions.”
Before establishing the adult neuro-ophthalmology program at ChristianaCare, patients in Delaware often had to travel to Pennsylvania or Maryland, facing logistical and insurance challenges. Now, ChristianaCare provides these specialized services locally, eliminating the need for out-of-state travel.
“Now, we can serve the community and reduce barriers to care. It’s rewarding to know I’m making a difference,” said Dr. Fraz.
The new program actively collaborates with subspecialties across neuroscience and ophthalmology, including headache, neuroimmunology, neuro-interventional surgery, neurosurgery, retina, glaucoma and oculoplastics. Temple University ophthalmology residents also rotate in the Neuro-Ophthalmology Clinic as a part of their training.
“Working closely with colleagues in both neurology and ophthalmology enhances the care we provide,” Dr. Fraz noted.
Beyond ophthalmology, Dr. Fraz actively collaborates with other subspecialists within the ChristianaCare system. A notable example is his partnership with the neurointerventional surgery team and neurosurgery to address idiopathic intracranial hypertension (IIH), a condition that predominantly affects young to middle-aged individuals, primarily women. Patients with IIH often experience symptoms like headache, vision loss, pulsatile tinnitus and double vision due to increased intracranial pressure. This collaboration includes venous sinus stenting with neurointerventional surgery and ventriculoperitoneal shunting with neurosurgery, streamlining the patient’s treatment journey within ChristianaCare.
“In cases where medical treatment is insufficient, surgical interventions may be necessary to preserve vision,” Dr. Fraz explained. “We’re proud to be growing and bringing something new to the state. All great things have to start somewhere.”
The novel magnetic resonance (MR)-guided focused ultrasound technology allows for tremors to be controlled without surgical incisions, meaning that patients can experience immediate results with minimal to no recovery time. At ChristianaCare, the first MR-guided focused ultrasound procedure was performed on June 6, 2024. Since that time, the team has completed nearly 20 procedures.
“We’ve ramped up a lot more quickly than expected,” said Justin Martello, M.D., the director of the Parkinson’s and Movement Disorders Programs and Focused Ultrasound Program at ChristianaCare Neurology Specialists.

Although the initial plan was for the team to conduct approximately four MR-guided focused ultrasound procedures per month, the success of, and demand for, the procedure meant goals were quickly revised.
“After the first month and a half, when we saw how successful the program was and how dramatically it was improving these patients’ lives, we increased the frequency of the procedures to two per week,” Dr. Martello said.
In addition, exciting developments regarding focused ultrasound are being tested in clinical trials, likely meaning that the procedure will be able to be used in new and innovative ways in the near future. The first, which Dr. Martello noted will likely occur by the end of the first quarter of 2025, is a new indication to use the technology to treat other symptoms of Parkinson’s disease, such as slowness and stiffness of movement and dyskinesia. By mid-2025, another new indication may expand the use of focused ultrasound even further; specifically in the area of cancer diagnostics.
“This current treatment is technically considered high-intensity focused ultrasound,” Dr. Martello clarified. “And an indication for low-intensity or low-frequency ultrasound is likely.”
Whereas high-intensity ultrasound uses heat from wavelengths to target and kill specific areas of the brain that are responsible for causing tremors, low-intensity ultrasound does not heat up the brain tissue. Instead, the technique safely breaks open the blood–brain barrier for a brief period of time—often 1.5 to two hours—allowing unprecedented access to regions of the brain.
“When a patient has a tumor in their brain, often it isn’t possible to do surgery in order to either conduct a biopsy or remove the tumor due to its deep position in the brain,” Dr. Martello said. “This technique, which is called liquid biopsy, opens up the blood–brain barrier and stimulates blood flow around the tumor.”
This can slightly break up the tumor, allowing its cells to circulate in the blood. Doing so means doctors can take a blood sample, which will contain cancer cells that can then be tested in order to complete a diagnosis without necessitating surgery or traditional biopsy. While breaking up pieces of the tumor can aid in diagnosis, it does not result in spreading of the cancer to other areas of the body.
“What it does do is allow for a noninvasive way to diagnose the cancer that doesn’t risk permanent damage to the brain,” Dr. Martello said.
The technique may also allow for novel ways of delivering medications that aren’t normally able to cross the blood–brain barrier, potentially offering benefits for patients undergoing chemotherapy, as well as those receiving treatment for conditions such as Alzheimer’s disease.
These developments, Dr. Martello says, will help to both increase the use of this cutting-edge technology and allow for more neurologists to offer the benefits of focused ultrasound to their patients.
The goal of a scheduled EMU admission for a patient is to characterize and localize the seizure-like event so that the appropriate diagnosis can be made and treatment can be initiated. Many patients treated in the EMU are there for preoperative evaluation before surgery designed to control seizures, if pharmacotherapy has failed.
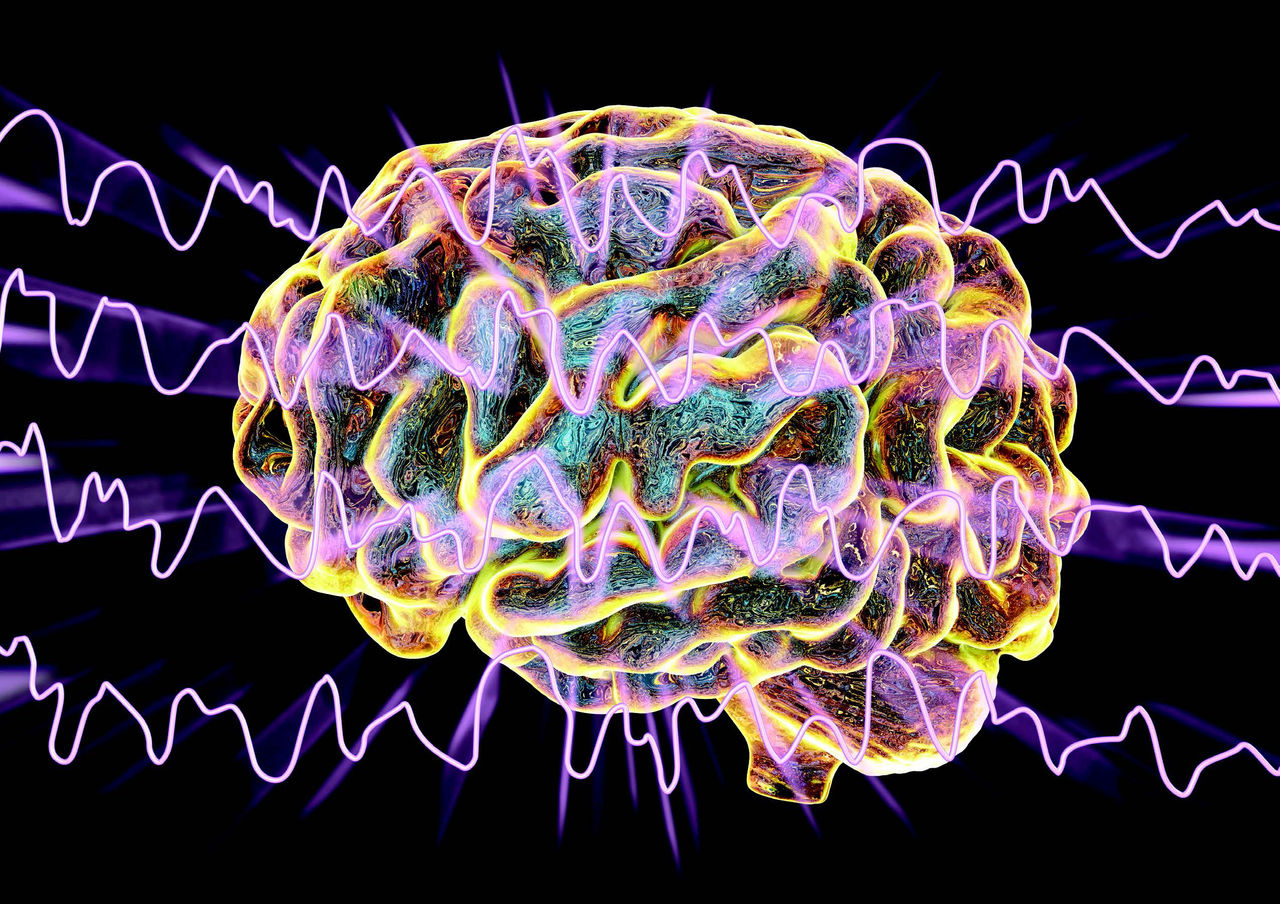
The EMU is a specially equipped inpatient unit that uses continuous EEG monitoring, continuous video monitoring through ChristianaCare Virtual Health and continuous heart rate monitoring, according to John Pollard, M.D., an adult epileptologist and the director of the Epilepsy Center at ChristianaCare. The EMU strives to provide a superior level of for complex epilepsy patients and accredited by the National Association of Epilepsy centers as a Level 3 center. Level 3 centers provide a range of neurodiagnostic evaluations and medical, neuropsychological, and psychosocial services needed to diagnose and treat patients with refractory epilepsy. Between 50 and 100 patients visit the unit annually.
“When someone has a seizure in our EMU, the nurse can come in and care for the patient and perform an assessment called an ictal cognitive exam,” Dr. Pollard said. “This combination of factors—the video, the ictal cognitive exam and the EEG exam—is very effective at determining what kind of seizures people are having.”
“In the EMU, we do presurgical evaluation; we do differential diagnosis to capture a seizure episode and make the right diagnosis, and we also use the EMU to adjust medications occasionally,” noted June Wang, M.D., PhD, an adult epileptologist and EEG lab director at the Christiana Hospital.
At least half of the people who go into the EMU at ChristianaCare don’t know why they are having seizures, and some of them turn out to be having events that are not actually epilepsy but the result of some other cause, such as a psychological problem or a heart arrhythmia that leads syncope. In some cases, a patient’s seizures are determined to be from a transient ischemic attack.
“We want to see if someone is eligible for an epilepsy surgery by trying to discover whether it would be safe to take out the spot or spots in their brain that is causing the seizures,” Dr. Pollard noted.
The EMU has also instituted what its specialists call a fall prevention system to limit the risk for the 1 in 10 epilepsy patients (national average) who experience a fall in the hospital.
“Our fall prevention system has been adapted from the system used by physical medicine and rehabilitation,” Dr. Pollard said. “It’s a vest that attaches to the bed lift, so if someone has a fall, then they don’t actually hit the ground because the vest stabilizes them. Uniquely, in our EMU, falls are incredibly rare.”
Because of these and other innovations, ChristianaCare’s Epilepsy Center of Excellence is prepared to care for a range of patients with epilepsy and seizure-like events, including those with special needs. In addition, the health system’s pharmacy has a protocol for pregnant women who often need their epilepsy medications adjusted; pregnancy alters blood levels of certain medications, placing women at increased risk for seizures.
To expedite appropriate care, the epilepsy team has developed and instituted an uncomplicated seizure pathway that provides quick treatment access to patients who present to the emergency room with seizures, and newly diagnosed patients with epilepsy are offered education and expedited ambulatory appointments. The ChristianaCare Epilepsy Center of Excellence also works closely with neuropsychology and neuroradiology to ensure accurate diagnoses, and with neurosurgeons to provide on neuromodulation therapy, if applicable.
To address this issue in New Castle County, home to 60% of Delaware’s population, ChristianaCare has partnered with the county’s emergency medical services (EMS) to become an early adopter of Twiage, a novel prehospital communication and intrahospital care coordination technology. The system is designed to facilitate communication between hospital personnel and EMS to accelerate lifesaving emergency care by reducing dependence on radio communication.
Twiage is available to EMS personnel for free, and the HIPAA-compliant app can send notifications with patient vital signs, symptoms (including EKG results) and interventions to the hospital in seconds, along with photos, additional details in text chats and digital voice memos. That information is readily available to health-system vascular neurologists on their cellphones, according to Kim Gannon, M.D., Ph.D., the medical director of ChristianaCare’s Comprehensive Stroke Program and physician executive of the Neurosciences Service Line.
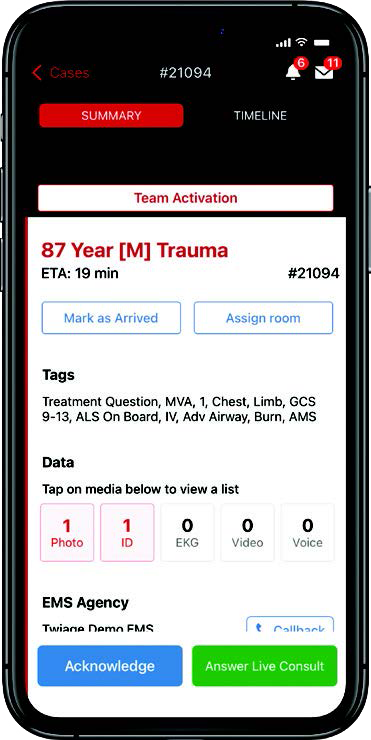
“When neurologists can have that information available, prior to the patient’s arrival at the hospital, it can make all the difference in the world because seconds truly matter in stroke care,” said Dr. Gannon. ChristianaCare’s stroke program is one of the largest nationally and one of only 300 comprehensive centers across the country. “With this system, paramedics can communicate with our stroke teams while they’re on their way to the hospital, which gives our staff time to access and review the patient’s chart. This is particularly important if the patient is unable to speak for themselves or doesn’t have a family member present.”
Research suggests that stroke patients lose approximately 1.9 million brain cells per minute during care delays, making rapid initiation of antithrombotic therapy crucial, added Doug Huisenga, the senior program manager for ChristianaCare’s systemwide stroke program. However, although these drugs are widely used and effective, there are contraindications in many patients, including a history of cerebral hemorrhage and/or ischemic stroke (within the past three months).
“That’s why having access to a patient’s personal health information is so important,” he said.
Efficient stroke care represents a particularly acute need in Delaware, which is actually located in the northernmost reaches of the so-called “stroke belt,” the region comprising most of the Southeastern United States that has the highest incidence of stroke mortality in the country. The state actually has the second-highest incidence of stroke mortality (56.8/100,000 people in the general population) in the country, behind Mississippi.

Of note, hypertension and hyperlipidemia as well as tobacco use are very common in Delaware. ChristianaCare is the only comprehensive stroke center on the I-95 corridor between Baltimore and Philadelphia.
The initiative with New Castle County EMS and ChristianaCare means Delaware is now one of 12 states nationally in which the Twiage system is in use. By providing patient data and GPS-tracked ETA for all incoming ambulances in real time, Twiage helps reduce hospital efficiency and enables earlier initiation of treatment, meaning lives are saved.
“ChristianaCare is already likely in the top 1% of hospitals nationally in door to needle time,” said Huisenga, referring to the initiation of antithrombotic treatment. “However, one of the ways we can make that even better is to improve prehospital communications — and that’s what we’ve done with Twiage thanks to this collaboration with New Castle County EMS.”
Cutting-edge magnetic resonance (MR)-guided focused ultrasound technology is allowing neurologists at ChristianaCare to provide outpatient procedures for patients struggling with essential tremor (ET) and Parkinson’s disease.
Developed in the early 2000s, and approved by the FDA in 2016, the technique allows for tremor control without surgical incisions, meaning that patients can recover quickly, are not at risk of destabilizing infections and are able to experience immediate reduction of their tremors. This summer, Justin Martello, M.D., the Parkinson’s and movement disorders director at ChristianaCare Neurology Specialists, will use the technology for ET and Parkinson’s patients as the first in the state of Delaware to offer this treatment.
In focused ultrasound, MRI is used to develop a detailed picture of a patient’s brain. Ultrasound wavelengths are then used to heat and kill the specific cells responsible for causing the individual’s tremors, essentially creating a lesion in the region of the brain.
“We can pretreat the region at low levels of heat energy without causing any damage,” Dr. Martello said. “This stuns the cells. We can then review the MRI and ask the patient how they are feeling.”
Adding to the procedure’s safety is the fact that it can be nondestructively tested and guided by immediate patient feedback, according to Dr. Martello. In ET patients, the procedure can be done on both sides of the brain — albeit in separate treatments about nine months apart — to achieve full relief from tremors affecting both sides of the body.
“If the tremor is still there or the patient has side effects, we know we are not in the right spot, but we haven’t done any permanent damage so we can move on to a different area,” Dr. Martello noted. “By doing that, we can make sure we are treating the correct area and avoiding side effects.”
Essential tremor is the most common movement disorder in the United States, affecting an estimated 6.4 million people.1 The disorder typically occurs later in life and is an inherited condition in up to 70% of patients.2
“Everyone has a tremor center of their brain,” Dr. Martello explained. “For patients with tremors it is not functioning correctly.”
Focused ultrasound has been found to be very effective for tremor. A study published in The New England Journal of Medicine in 2016 determined that patients’ mean scores for hand tremor improved by 47% at three months in the cohort receiving the treatment, compared with 0.1% in study participants who underwent a sham procedure.3 And the noninvasive nature of the technique makes it particularly appealing for older patients who may be poorly suited for an invasive approach.
“The results can be dramatic,” Dr. Martello said. “Patients who have been living with this for decades are able to come out of the procedure and drink from a glass.”
Dr. Martello and team will select a very specific area of the brain to create a small lesion to decrease or eliminate the tremor. They have to weigh treating a larger area of the brain for more tremor reduction against possible increased risk of side effects.
Recent five-year data have been promising, showing that Clinical Rating Scale for Tremor scores significantly improved by 73.3% and 73.1% from baseline at both 48 and 60 months post-treatment, respectively.4
“Back in the day, we wanted to treat the whole tremor so we did big lesions, but we saw side effects such as balance issues,” Dr. Martello said, adding that correcting this behavior has caused some surgeons to create too small of a lesion, which may allow for the tremors to return. “Trying to find a middle ground of treating enough of the involved cells, but not so much that you are getting side effects.”
References
- Crawford S, Lally C, Petrillo J, et al. How many adults in the US have essential tremor? Using data from epidemiological studies to derive age-specific estimates of prevalence. Neurology. 2020;94(15 suppl):4458.
- Lorenz D, Frederiksen H, Moises H, et al. High concordance for essential tremor in monozygotic twins of old age. Neurology. 2004;62(2):208-211.
- Elias WJ, Lipsman N, Ondo WG, et al. A randomized trial of focused ultrasound thalamotomy for essential tremor. N Engl J Med. 2016;375(8):730-739.
- Cosgrove GR, Lipsman N, Lozano AM, et al. Magnetic resonance imaging-guided focused ultrasound thalamotomy for essential tremor: 5-year follow-up results. J Neurosurg. 2022;138(4):1028-1033.
A patient diagnosed with multiple sclerosis (MS) 20 years ago would have faced significant disability, pain, and perhaps a shortened life span.
Although there’s currently no cure for the neurologic disorder, which typically occurs in young adults aged 20 to 40 years, neurologists at ChristianaCare are embracing new treatments designed to help manage the course of the disease and limit its disabling effects. Treatments include disease-modifying therapies (DMT), which can slow disease progression and relieve some symptoms.
“The best practice in managing a patient’s MS is through a multidisciplinary team approach that meets both the medical and nonmedical needs of patients, during any stage of the disease,” said Xiaoyang Li, M.D., a neuroimmunologist at ChristianaCare. “Our patients are guided through different treatment options during all stages of their lives, including instruction for patients and families about medicines and how to best manage symptoms.”
Indeed, ChristianaCare’s MS Comprehensive Center of Excellence provides the most effective advanced treatments and symptom management approaches available. Today, MS is considered a chronic disease that is manageable. If it’s diagnosed early and treatment is initiated before symptoms progress, patients can maintain function for years.
With immunotherapies such as DMTs, patients who start treatment early in the disease course can lead relatively normal lives. In MS, the immune system attacks healthy tissue and nerve cells in error, causing muscle weakness and movement problems. DMTs work by lowering the activity of the immune system, limiting its ability to attack healthy cells. In many patients, these drugs alter the course of MS, reducing their risk for disease relapse, decreasing disease activity and slowing symptom progression.
The FDA has approved more than a dozen DMTs for different types of MS, including clinically isolated syndrome, relapsing-remitting, secondary progressive and primary progressive. However, the drugs have proved most effective in treating the first three types.
Most of the DMTs recommended by neurologists within ChristianaCare’s MS Comprehensive Center of Excellence are infusion-based and can be administered in six-month dosing schedules. Because of a range of choices depending on the patient’s type of MS, treatments can be tailored for a specific patient, allowing for better disease management.
Still, although DMTs offer increased efficacy, often with fewer side effects than more traditional treatments, they do not reverse any nerve damage caused by MS that occurred prior to diagnosis.
Even with these advances, “the most important consideration in the overall management of MS is an early diagnosis and early treatment intervention with the most advanced therapies available,” Dr. Li said.
“On a daily basis, my colleagues and I treat disorders of the blood vessels in the head, neck and spine — aneurysms being one of them,” said Barbara J. Albani, M.D., the medical director for neurointerventional surgery at ChristianaCare. “Given the wide array of devices and techniques that are at our disposal we are able to tailor treatment specifically to each individual patient.”

Of these techniques, endovascular coiling is the oldest, dating back to the 1990s. The procedure involves the use of small, flexible catheters that are typically inserted via a patient’s femoral artery. Once the catheter has reached the brain, the surgeon is able to place coils in the aneurysm.
Platelets adhere to the coils and heal in a way that restricts blood from reaching the out-pouching of the aneurysm.1
“This is a very sophisticated way to treat an aneurysm without having to open up the patient’s head and displace their brain,” Dr. Albani said. “Everything is done from within the artery without causing any disruption to the brain tissue.”
Although the technique works on saccular aneurysms — those with a lollipop or mushroom-like shape — others, which are fusiform or wide-necked in shape, require alternative approaches. For these, an open celled stent can be used which has gaps that can be crossed by a wire or a microcatheter, but will hold coils into an aneurysm. The stents are placed in the parent artery near the aneurysm, and a guidewire is passed through the stent in order to place coils within the aneurysm.
“Once placed, the stents help buttress the coils in order to keep them from falling out,” she said.
For certain patients, a finer mesh stent may be used, according to Dr. Albani. These permeable, flow-diverting stents are made of a very fine-gauge mesh that looks similar to a woman’s stocking.
They act to divert blood away from the aneurysm.
“Blood can still seep in, but it is not driving into the aneurysm,” Dr. Albani said. “The analogy I use for patients is it’s kind of like a coffee filter — the water will pass through but not flow with abundance. And the more filters you put in, the less flow you get through it. Over time, the body will endothelialize; the lining of the vessels will grow over the flow-diverting stent, remodeling the blood vessel and effectively sealing it from the inside.”
More recent technologies include the Woven EndoBridge WEB Embolization System (MicroVention) and the Contour Neurovascular System (Stryker).
“The WEB system looks almost like a square ball of yarn and keeps blood from getting into the aneurysm,” Dr. Albani said.
The Contour system, which Dr. Albani noted is shaped like an umbrella that has been inverted by the wind, can be inserted into an aneurysm and cinched down in order to serve as a wall that coils can be inserted behind. Indicated for wide-necked aneurysms, neither system uses a stent, meaning nothing needs to be placed in the parent artery, negating the need for antiplatelet medications that may not work for all patients.
“Whenever we put a stent into somebody’s artery, we have to put them on antiplatelet medications, and this usually involves keeping them on aspirin for life,” Dr. Albani said. “These devices can be a godsend for patients who can’t take aspirin, or who for other reasons we don’t want to put on blood thinners.”
Key to the ChristianaCare team’s approach is a deep understanding of, and experience with, each of the techniques, allowing them to customize each patient’s care.
“We have been early adopters of all of these things, have lots of experience using them and can tailor a patient’s treatment to what they need,” Dr. Albani said. “We have everything we need to make sure the patients are covered, and are here 24/7/365 to help with questions or concerns.”
References
- Ogilvy CS. Neurosurgical clipping versus endovascular coiling of patients with ruptured intracranial aneurysms. Stroke. 2003;34(10):2540-2542.
Patients receiving care in the Neurocritical Care Unit at ChristianaCare with concern for seizure may benefit from a new electroencephalographic (EEG) technology on-boarded by health-system neurologists.
The platform, called Ceribell® EEG (by the manufacturer of the same name), enables rapid evaluation of possible seizure activity when a standard EEG is not immediately. The technology enables ChristianaCare neurologists to quickly evaluate for seizure activity even when EEG technicians are not immediately available.
“This tool allows us to obtain a diagnosis quickly and initiate treatment as needed,” explained Huijun Wang, Ph.D., a specialist in neurology and psychology at ChristianaCare. “It doesn’t have the same sensitivity and specificity as traditional EEG, but it gives us enough information to confirm or rule out seizure in minutes, when we need it, in an emergency situation. That, combined with clinical suspicion, can be enough for us to begin treatment.”

For patients with suspected seizure, time to diagnosis is a key determinant of outcomes, similar to the door-to-needle times in the management of ischemic stroke, as indicated by research. The sooner neurologists can start antiseizure treatment in patients, the more likely they can keep the brain disorder under control.
The primary benefit of Ceribell’s Food and Drug Administration-approved EEG device is that it is completely automated and can be operated by doctors and nurses at the bedside, without a specialized EEG technician, after minimal training. The device is a reduced-montage (8-channel) circumferential EEG that produces tracings covering the frontal, temporal and occipital areas. During evaluation, electrodes are implanted in a soft, adjustable headband attached around the head and secured for electrode grip, and amplified brain signals are transmitted to a pocket-sized device that allows patient data to be entered and viewed in real time.1
Currently, the technology is being used by neurologists as well as nurses and advanced care practitioners in the neuro-ICU at ChristianaCare’s ewark facility. Pending results, it may be expanded to other facilities later this year.
In studies, Ceribell® EEG has been shown to significantly reduce time to diagnosis. A recent analysis published in the journal Epilepsia Open found that mean time to epilepsy diagnosis with the device was 23.8 minutes.2 In her experience with the technology, though, Dr. Wang said it can essentially provide diagnostic information in “real time.”
With that said, Ceribell® EEG doesn’t — and won’t — replace conventional, state-of-the-art EEG platforms, which are more accurate and provide a more complete reading of electrical activity in the brain, according to Richard K. Choi, D.O.. Many patients initially evaluated with the novel device will undergo conventional EEG later to confirm early findings, he said.
“Ceribell® EEG is really like the farmer’s dog barking in the middle of the night — it can warn us that something is or is not happening in a patient’s brain; but the farmer, or in this case the neurologist, will still need to confirm whether it’s something serious,” explained Dr. Choi, a neurologist and neurocritical care specialist at ChristianaCare. “Our use of this technology really highlights ChristianaCare’s ability to see a challenge and find an effective way to address it. It really reflects our values and behaviors, one of which is making sure we’re using all resources available to ensure the best care for our patients.”
References
- Parvizi J, Gururangan K, Razavi B, et al. Detecting silent seizures by their sound. Epilepsia. 2018;59(4):877-884.
- LaMonte MP. Ceribell EEG shortens seizure diagnosis and workforce time and is useful for COVID isolation. Epilepsia Open. 2021;6(2):331-338.
Botox (onabotulinumtoxinA, Allergan) injections have emerged as the most effective option for the treatment of chronic migraine, and specialists at ChristianaCare were early adopters of the innovative approach.
Botox is a neurotoxin that, when injected into muscle tissue, can prevent movement of the treated muscle for a limited time. Best known as a treatment for smoothing wrinkles in the skin on the face, these injections have traditionally been used to treat neuromuscular issues, including spasms and other muscle-contracting conditions.
“In addition to being the most effective treatment we have for refractory chronic migraine, Botox doesn’t have any systemic effects,” said Mitra Assidi-Khansari, M.D., a headache medicine specialist and the director of education in the Division of Neurology. “So, when we inject it into those tiny muscles on the cranial facial area, the medication basically remains in those muscles. It doesn’t float in your system, doesn’t affect the kidney or liver, and doesn’t penetrate your brain and cause cognitive side effects or changes in appetite or mood.”
Migraine headaches are extremely common, particularly in women. Up to 17% of women and 6% of men suffer from migraines.1 Chronic refractory migraine, in which patients experience frequent or long-lasting symptoms for 15 or more days per month, are somewhat less common than episodic migraine, in which patients have symptoms for less than 15 days per month.

As a result, the former “is, unfortunately, a very undertreated disorder,” noted Jessica Bradley, M.D., a headache medicine specialist ChristianaCare. “Many patients don’t seek care until the migraines have gotten bad enough that they are forced to seek treatment options.”
Botox was approved by the FDA in 2010 for use in the treatment of chronic migraine in adults with symptoms that have not responded to three other “standard treatments” (eg, calcitonin gene–related peptide antagonists and receptors). Based on the FDA guidelines, Botox can be administered every three months, for a total of four full treatments annually.
A standard protocol has been established for administering a total of 155 units of Botox. A recommended paradigm calls for injections on the frontal area, the temple, the occipital region over the cervical spinal area and on the top of the shoulders for a total of about 31 shots.
Botox exerts its effect mainly by decreasing signaling on the motor fibers and reducing muscle tension in the cranial facial areas. There are some theories indicating that it can also disrupt the signaling on the sensory fibers.
In a study involving 245 patients with migraine, 82.9% reported that Botox helped control their symptoms.2
Despite its effectiveness, patients need to set expectations on what to anticipate from Botox treatments.
“The first thing I tell patients is that the treatments often don’t work in the first session,” Dr. Bradley said. “Botox treatments often have a cumulative build up in effect, and it can take up to three rounds of treatment to reach maximum migraine control. I explain this to my patients before starting so they know what to expect and won’t feel discouraged if the first treatment does not work well. I encourage patients to try at least three rounds of Botox before determining its effectiveness.”
References
- Stewart WF, Shechter A, Rasmussen BK. Migraine prevalence. A review of population-based studies. Neurology. 1994;44(6 suppl 4):S17-S23.
- Yalinay Dikmen P, Kosak S, Ilgaz Aydinlar E, et al. A single-center retrospective study of onabotulinumtoxinA for treatment of 245 chronic migraine patients: survey results of a real-world experience. Acta Neurol Belg. 2018;118(3):475-484.
Heart & Vascular
Early in 2025, vascular surgeons at ChristianaCare’s Center for Aortic Health performed Delaware’s first-ever Gore TAMBE, or Thoracoabdominal Multibranch Endoprosthesis, a novel, minimally invasive approach for the surgical management of complex abdominal aortic aneurysms that uses an off-the-shelf aortic stent graft for endovascular repair.
This new technology is the first FDA-approved, off-the-shelf endograft for the endovascular repair of complex thoracoabdominal aneurysmal disease involving the visceral aorta. Thoracoabdominal aortic aneurysms (TAAAs) involve the segment of the aorta from which critical branches originate, including the arteries supplying the liver, intestines, kidneys, and spinal cord.

Repairing aneurysms or dissections in this region requires maintaining blood flow to these organs while simultaneously rebuilding or reinforcing the aorta. Traditionally, such repairs required large, open surgeries with significant risk and prolonged recovery.
“Completing the first few TAMBE operations in Delaware marks an important milestone for patients who, until now, had no local option for this level of care,” said Kathryn E. Bowser, M.D., a Vascular Surgeon at the Center for Aortic Health at ChristianaCare who led the first TAMBE procedure. “TAMBE enables us to treat thoracoabdominal aneurysms with a multibranch endograft that maintains flow to the visceral arteries. Through advanced technology, meticulous planning, and deep expertise, we can today repair these life-threatening problems in a minimally invasive fashion.”
Unlike traditional thoracic stent graft devices, which need to be customized in the operating room for each individual patient and inserted via complex, open procedures, the TAMBE device is placed percutaneously via the femoral and axillary arteries, using small incisions in the groin and arm.
The device itself is a collapsed, multibranched stent graft that is inserted through the groin and, with real-time image guidance, is navigated through the blood vessels to the aneurysm. Once in the aorta, it expands to line the artery and seal the aneurysm, preventing a rupture. Its built-in branches are then connected to the arteries that supply blood to the kidneys, liver, intestines, and other organs.
“The goal of the TAMBE device is to have an off-the-shelf endovascular solution for TAAAs that can work in a large percentage of patients,” said ChristianaCare vascular surgeon Mikael Fadoul, M.D., who was part of the surgical team that performed the first TAMBE procedure in Delaware. “With TAMBE, we don’t have to custom order a device or put patients through complex, open surgery, which has a very high morbidity and mortality.”
The TAMBE device adds to the surgical armamentarium available to vascular surgeons at the Center for Aortic Health, all of whom have vast experience with physician-modified fenestrated endografts (PMEGs) for complex aneurysm anatomy, including TAAAs, and perform these procedures routinely.
“PMEGs are redefining what is possible for patients who previously had limited options,” Dr. Bowser said. “They allow us to tailor fenestrations or branches to each patient’s anatomy. These modifications require extreme precision, device knowledge, and intraoperative adaptability. They enable the safe treatment of complicated aneurysms in patients who are not candidates for standard devices.”
Surgical management of complex aortic cases requires significant coordination, teamwork, and planning, according to Dr. Bowser. The process begins with detailed computed tomography–guided reconstruction and measurement, and includes device planning and customization, collaboration with device manufacturers, spinal cord protection strategies, and contingency plans for multiple anatomic scenarios. These procedures engage a multidisciplinary team that includes vascular and cardiac surgeons, the operating room vascular team, anesthesiologists, intensivists, genetic specialists, cardiologists, and others.
“Because no two aortas are identical, each plan is tailored. In some cases, an endograft needs to be hand-modified the day of surgery itself—an intricate, high-stakes technical process that requires very advanced training and continuous attention to detail,” Dr. Bowser said. “On the day of surgery, success depends on a smooth interplay among several disciplines. Our hybrid operating rooms and vascular specialists function as one single unit, ensuring precision with complex arterial access, wire and catheter techniques, precise device deployment, branch vessel catheterization and stenting, neurologic monitoring, and real-time imaging interpretation, as well as management of possible complications like endoleaks, dissections, or branch occlusion.”
The addition of TAMBE to this expertise means patients diagnosed with a TAAA at ChristianaCare have a new lifesaving option.
“Bringing this level of aortic care to Delaware has a profound impact,” Dr. Bowser said. “Patients can stay closer to home, near their families, support systems, and familiar health care environment. Emergency cases can be treated more quickly, and survival can be improved in time-sensitive scenarios. This type of innovation makes ChristianaCare a regional leader, enabling us to take complex referrals while elevating cardiovascular care statewide.”
For patients suffering from painful or chronic hemorrhoids, a new minimally invasive procedure is offering relief without the need for surgery. At ChristianaCare, interventional radiologists are now performing hemorrhoidal artery embolization (HAE), or the emborrhoid technique, an innovative treatment that’s transforming care for patients with moderate hemorrhoidal disease.
“Symptomatic hemorrhoidal disease is a prevalent condition that significantly impacts patients’ quality of life,” said Christopher Grilli, D.O., F.S.I.R., an interventional radiologist at ChristianaCare.
Traditional treatment approaches for the condition range from conservative management to invasive surgical procedures such as hemorrhoidectomy.

“In recent years, HAE has emerged as a promising minimally invasive alternative, particularly for patients with Grade II or III internal hemorrhoids who are not optimal surgical candidates or prefer a less invasive approach,” Dr. Grilli said. “With HAE, we can offer patients a kinder, gentler option, a nonsurgical procedure that provides excellent results, minimal discomfort, and a quick return to normal activity.”
Before the procedure, patients undergo a detailed clinical and proctologic examination, often accompanied by a colonoscopy or sigmoidoscopy to rule out other causes of rectal bleeding. In selected cases, a pelvic MRI or CT angiography may also be performed to better define the vascular anatomy.
“Most patients we see have been dealing with hemorrhoids for quite some time, often with bleeding or pain that hasn’t responded to other therapies,” Dr. Grilli explained. “We want to make sure we fully understand what’s going on and that HAE is the right fit for them.”
HAE works by targeting the blood vessels that supply the hemorrhoidal tissue. A small catheter is inserted through a pinhole access point under x-ray guidance, either in the wrist or groin, and advanced to the arteries feeding the rectal area. Tiny metal coils are then used to block blood flow to the hemorrhoids, allowing the dilated veins to shrink and symptoms to resolve.
The process is performed under local anesthesia with moderate sedation, and a post-embolization angiography confirms successful devascularization. The procedure is quick, safe, and minimally invasive—and recovery is far faster than it is for surgical approaches.
“The entire procedure takes about 45 minutes to an hour,” Dr. Grilli said.
Patients are able to go home the same day, and most can resume normal activity within 24 to 48 hours. Because HAE does not disturb the anal or rectal anatomy, it also preserves normal function and continence, an important consideration for patient quality of life.
Results from published studies, as well as clinical experience, show that HAE is effective and offers durable results.
“About 80% to 90% of patients report improvement in symptoms within a week, and bleeding often resolves in just a couple of days,” Dr. Grilli said. “This is where HAE really shines compared to surgery, which can involve a recovery of one to two weeks depending upon how it is done.”
Additionally, the safety profile of HAE is excellent. There is minimal risk for infection or complications, and while most patients report sustained relief and low recurrence rates, the procedure can be repeated if and when symptoms return.
“HAE represents a significant advancement in the treatment of hemorrhoidal disease,” Dr. Grilli said. "As clinical experience and evidence grow, HAE is poised to become an integral part of the treatment algorithm for select patients.”
Endometriosis occurs when tissue similar to the uterine lining grows in the muscle of the uterus or outside of the uterus. While this growth can occur in other areas, it is most frequently found in the pelvis.
“This is the tissue that is shed with menstruation—it just happens to be in the wrong spot,” said Michelle Pacis, M.D., a minimally invasive gynecologic surgeon at ChristianaCare. “Endometriosis causes inflammation, which can result in significant pain and can also affect reproductive anatomy thereby causing infertility issues depending on where it’s located.”

While medications such as hormonal therapy can help control symptoms, and surgery remains the gold standard for diagnosis and treatment, many patients face a long road before receiving an accurate diagnosis.
“Endometriosis affects about 10% of women, and it takes an average of five to 10 years for someone to be diagnosed appropriately,” Dr. Pacis said. “People are often told that painful, heavy periods are normal, and their concerns may be dismissed for years.”
In rare cases, endometrial tissue can implant into the abdominal wall, often in the scar from a previous cesarean delivery or laparoscopic procedure.
“These lesions can be particularly painful,” Dr. Pacis said. “Traditionally, the only way to treat them has been surgical excision, which can be invasive, create additional scarring, and require a longer recovery period. That’s where cryoablation is offering a real breakthrough.”
Cryoablation is a technique that was invented in the mid-19th century and involves using extreme cold to destroy abnormal tissue via precisely targeted freezing.
“The procedure has been well established for treating tumors in the kidneys and lungs as well as other soft-tissue tumors,” said Christelle Chedrawy, M.D., a vascular interventional radiologist at ChristianaCare. “More recently, cryoablation has been applied to endometriosis of the abdominal wall, with promising results.”
Cryoablation is performed under imaging guidance—using ultrasound, CT, or both—and patients are given either local anesthesia with moderate sedation or general anesthesia, if needed.
“We insert thin probes directly into the lesion under imaging guidance,” Dr. Chedrawy said. “The number of probes depends on the size of the lesion. We confirm that we’re away from nearby structures such as the bowel, sometimes using an injected solution to create a protective barrier. Once everything is positioned safely, the standard freeze-thaw-freeze cycle is 10-8-10 minutes.”
The visibility of cryoablation is a significant benefit.
“The ice ball that forms around the targeted area is visible on CT and ultrasound, so we can monitor it in real time,” Dr. Chedrawy said. “That allows us to ensure complete coverage of the lesion while protecting surrounding organs.”
The entire process for the procedure takes roughly two to four hours. Patients are observed for several hours afterward and are usually able to go home the same day.
“I usually do a follow-up in one month to see how patients are doing,” Dr. Chedrawy said. “Because endometriosis tissue behaves differently than other tumors, patients may have bruising and discomfort for a couple of weeks, but most report significant improvement by the one-month visit.”
While cryoablation for abdominal wall endometriosis is still a relatively new offering, early data are encouraging.
“Published reports, though based on small patient populations, show that cryoablation is safe and effective, with a primary efficacy rate of around 90%. The median pain-free survival rate at six months has been reported to be around 93%,” Dr. Chedrawy said. “For patients who are not surgical candidates or wish to avoid another operation, this offers a minimally invasive, image-guided option with a quick recovery.”
Dr. Pacis agreed that the technique fills an important gap in care for patients with endometriosis. The team at ChristianaCare, which included minimally invasive gynecologic surgeons as well as vascular interventional radiologists, performed its first cryoablation for abdominal wall endometriosis in March 2025, with positive results as of the six-month follow-up.
“This is a great collaboration between the two services and it has really changed patient’s life,” Dr. Chedrawy said.
“Abdominal wall endometriosis is uncommon—affecting about 1% of patients with endometriosis—but it can cause severe pain, particularly when associated with cesarean section scars,” she said. “This approach provides a less morbid alternative to surgical resection, helping patients avoid another incision and another scar.”
Innovations in the treatment of tricuspid regurgitation (TR) now allow for minimally invasive procedures that avoid the need for open-heart surgery. ChristianaCare’s Center for Heart & Vascular Health is one of the first institutions in the country to offer tricuspid valve repair or replacement using two new FDA-approved percutaneous catheter–based procedures.
“These procedures are not surgery. They are performed by threading small pieces of equipment through the veins and into the heart,” said Erin Fender, M.D., an interventional cardiologist at the Center for Heart & Vascular Health. “The entire procedure is done through an IV placed in the vein at the top of the hip bone. After the procedure, patients do not have an incision; there is only a small bit of surgical glue over the IV site.”

TR causes less blood to flow to the lungs, leading the blood to back up behind the heart. This results in congestion of the kidneys and liver and significant fluid retention in the legs and abdomen.
The condition, which affects more than 1.6 million people in the United States, causes fatigue, shortness of breath, and kidney and liver damage. The most common etiologies of TR include long-standing atrial fibrillation, pacemakers, and congestive heart failure.
In the past, the impact of TR on patients was underappreciated, mostly because TR often occurs in tandem with other conditions, such as atrial fibrillation or heart failure. However, multiple studies have shown that TR is independently associated with poor patient outcomes.1
Previously, open-heart surgery was the only option to treat patients with significant TR; unfortunately, this was associated with significant risk. With the recent FDA approval of new devices, a novel pathway for treatment is now open, and studies have shown they can improve symptoms and reduce hospitalizations.2,3
ChristianaCare offers two minimally invasive procedures for patients with TR:
- TriClip (Abbott), which involves a staple clip that pulls the sides of the valve closer together to substantially reduce leakage; or
- EVOQUE (Edwards Lifesciences), which replaces the faulty tricuspid valve with a new tissue valve.
Patient and procedure selection are decided by a multidisciplinary team at the Center for Heart & Vascular Health to ensure that the right therapy is identified for each individual patient.
“ChristianaCare is one of the busiest hospitals on the East Coast, with extensive institutional expertise in the nonsurgical treatment of heart valve disease,” Dr. Fender said. “We are well equipped to embrace new technologies and are proud to be the only center in Delaware offering these therapies.”
Dr. Fender and her colleagues see these new tricuspid therapies as one of many important advancements in the field of minimally invasive heart valve therapy. The team at ChristianaCare is now able to offer nonsurgical interventions for all four cardiac valves, which may spare many patients from open-heart surgery.
“Structural cardiology is an evolving field, and the Center for Heart & Vascular Health will stay at the forefront and bring new therapies into practice to drive forward safer and less invasive treatments for our patients,” Dr. Fender said.
References
- Fender EA, Zack CJ, Nishimura RA. Heart. 2017;104(10):798-806.
- Sorajja P, Whisenant B, Hamid N, et al. N Engl J Med. 2023;388(20):1833-1842.
- Hahn RT, Makkar R, Thourani VH, et al. N Engl J Med. 2025;392(2):115-126.
Through facility acquisitions, expansions, and enhancements, the service line has grown its footprint along with that of the health system. The result is that patients in southern Delaware, as well as eastern Maryland and southeastern Pennsylvania, now have expanded access to ChristianaCare specialists across a wide range of disciplines.

“When I joined ChristianaCare 10 years ago, I would have said that the anticipated growth and expansion for the organization was primarily aimed at establishing better care within Delaware,” said Kirk N. Garratt, M.D., M.Sc., the medical director at the Center for Heart & Vascular Health and the John H. Ammon Chair of Cardiology at ChristianaCare. “That commitment hasn’t been diluted in any way, but the organization has come to understand the value of taking the ChristianaCare brand of care outside of the state.”
That expansion began in earnest with the health system’s 2019 acquisition of Union Hospital in Elkton, Maryland, which is located in Cecil County. At the time of the purchase, there were seven cardiologists serving the county and Union Hospital; however, following the COVID-19 pandemic, several of them left the community or stopped practicing entirely.
To address this need, ChristianaCare has, since 2023, permanently stationed a cardiologist and an advanced practice clinician with a specialty in cardiovascular care at Union Hospital and implemented a rotation of cardiologists from elsewhere in the system to support services Monday through Friday.
Early in 2026, the service line will have a second ChristianaCare Medical Group cardiologist provide regular support at Union Hospital. By 2027, “we anticipate expanding our presence to provide all inpatient and potentially all office-based cardiovascular services in Cecil County through the ChristianaCare Medical Group practice,” Dr. Garratt said.
In southeastern Pennsylvania, ChristianaCare entered a region that saw two hospital closures over the past decade. The health system purchased one of those hospitals, the 30-bed Jennersville Regional Hospital in West Grove, and rebranded it ChristianaCare Hospital, West Grove.
Rather than operating the facility as a “general hospital,” Dr. Garratt said, ChristianaCare has instead implemented a new approach to hospital-based care delivery called focused inpatient care, which provides specialized, highly targeted medical treatment tailored to a specific patient population or health need. At West Grove, the focus is now on the provision of care services associated with aging, including treatment of cardiovascular diseases.
Not far from the hospital, the Heart & Vascular service line opened a cardiovascular specialty practice embedded in a ChristianaCare primary care office staffed by cardiologist Ronald L. Lewis, D.O. This specialty practice will soon relocate closer to the West Grove hospital campus. The new practice location will have expanded clinical and diagnostic capabilities.
“There was so much demand for cardiovascular care in the area that as soon as we opened the practice about 15 months ago, Dr Lewis was swamped,” Dr. Garratt said. Demand is forecasted to increase as a result of the West Grove Hospital opening, and to make it easier for patients needing outpatient cardiovascular care, the practice is being moved to a building directly across the street from the hospital. For patients with more complex cardiovascular disorders, “we have a very efficient and low-friction transfer system between sites, so we can fast-track them over to our Wilmington campus or our Newark campus as needed,” he added.
Closer to home, so to speak, ChristianaCare has opened several physician practices in the past few years in Kent and Sussex counties in Delaware. Additional southern Delaware practice locations are in the planning stages. Focusing on primary care, these practices will bring enhanced services to communities such as Camden, Georgetown, Lewes, and Rehoboth Beach. The Heart & Vascular service line aims to support these practices with cardiovascular specialists. The plan is to eventually provide several of these practice locations with full diagnostic capabilities and perhaps ambulatory surgical centers to support cardiovascular procedures.
This growth is intended to ease access to cardiovascular care for patients throughout Delaware, eastern Maryland and southeastern Pennsylvania, including access to state-of-the-art treatments available at ChristianaCare Newark Campus. Advanced treatments include transcatheter aortic valve replacement, less invasive mitral valve repair, catheter-based tricuspid repair and replacement, pulsed-field ablation for atrial fibrillation, and renal artery denervation for refractory hypertension. Creating cardiovascular access points throughout Delaware also eases access to the only advance heart failure program in the state and multidisciplinary teams of peripheral vascular and aortic disease experts.
“At ChristianaCare, we have the ability to manage the most complex cases because we lean into some of the more advanced methods and approaches and have access to the most sophisticated technologies, and we achieve excellent outcomes thanks to our multidisciplinary approach,” Dr. Garratt explained. “Our expansion into these new areas means that we are bringing these services to places—and patients—that need them.”
“Patients who receive this type of LAAO only have a brief inpatient stay, about one night,” said Neil Wimmer, M.D., an interventional cardiologist and the director of Quality and Innovation at the Center for Heart and Vascular Health. “We’re even developing a protocol to send patients home the very same day as the procedure.”
During minimally invasive LAAO, cardiologists insert a device about the size of a quarter through a vein in the leg and into the left atrial appendage (LAA). Over time, tissue grows over the device and seals off blood from entering the LAA, preventing any blood clots from forming and protecting patients from stroke.
Studies support the efficacy of this procedure, showing that in patients at high thromboembolic risk, LAAO using the Watchman device has resulted in consistently low rates of stroke.1,2 Similar results have been reported using the Amulet device.3
Regarding which device they use, the ChristianaCare team decides based on the patient. They look at ultrasound imaging of the heart to understand the shape and size of the area being operated on.
“I think of it like going into a suit shop and getting fitted by the tailor for a special event. You don’t know exactly what size is going to fit until you get your measurements that day, and this is also true for LAAO,” Dr. Wimmer said. “We have a specialized team of experienced cardiologists and noninvasive imaging experts that performs the procedure.”
The Center for Heart and Vascular Health has been performing minimally invasive LAAO for about five years, with hundreds of procedures under its belt. Although there are risks involved during the procedure, such as damaging the heart itself or causing pericardial effusion, Dr. Wimmer noted these types of outcomes are quite rare.
While results from LAAO using these devices are positive, the ChristianaCare team is participating in a randomized trial studying additional protective benefits for stroke prevention in patients who receive LAAO and continue to take blood thinners compared with those taking only blood thinners.
For the approximately 12.1 million individuals in the United States living with AFib, minimally invasive LAAO is an important treatment advance. AFib is associated with a fivefold increase in the risk for ischemic stroke and accounts for an estimated 1 in 7 strokes overall. AFib causes more than 450,000 hospitalizations in the United States each year, with approximately 232,000 deaths.
Historically, patients with AFib did not undergo LAAO because it required invasive open-heart surgery. It was performed only in patients already undergoing open-heart surgery for other procedures. These patients could also take blood thinners, but there are known tolerability issues with this medication class.
“The need for this minimally invasive LAAO procedure has grown quite a bit in the past few years,” Dr. Wimmer said. “We actually had to create additional space in our facility to offer it to more patients.”
References
- J Am Heart Assoc. 2025;14(16):e039780.
- J Am Coll Cardiol. 2017;70(24):2964-2975.
- J Am Coll Cardiol. 2025;25(85):1141-1153.
Patients diagnosed with knee osteoarthritis experience significant pain that has a negative impact on their quality of life. A long-term solution through knee replacement is not an option for some patients; many are not candidates, and others opt out of surgery. These patient populations also may have osteoarthritis that does not respond to therapies such as anti-inflammatories or injectable pain relievers. As a short-term solution, injections require frequent visits to the doctor’s office.
Assaf Graif, M.D., a vascular interventional radiologist at ChristianaCare, and his colleagues on the vascular interventional radiology team, employ a novel technique for reducing knee pain in patients with osteoarthritis: genicular artery embolization (GAE). GAE is a minimally invasive intervention that targets the capillaries supplying the synovium.
"GAE is an excellent in-and-out procedure that provides long-lasting pain relief and allows patients to regain quality of life,” Dr. Graif said.
In GAE, a catheter is first inserted into the femoral artery and gently guided to the genicular arteries with the help of fluoroscopy. Iodine-based contrast is used to ensure that the catheter is placed properly (for patients with renal disease, there are other contrast options that are renal sparing). An interventional radiologist then meticulously selects each target artery in the joint, using the catheter to send particles into the designated capillaries.
When these abnormal blood vessels are embolized with embolic materials, the flow of blood, cytokines and other inflammatory proteins is disrupted. On average, patients experience improvement in pain levels after two weeks. With this single procedure, the benefits can be sustained for up to 24 months.
“Patients can return home two hours after the procedure has been completed,” Dr. Graif said. “They may experience temporary side effects, such as cramping and low-grade fever, which can be mitigated with ibuprofen and typically resolve within 24 hours.”
Patients also may see skin changes for a few days, he added, but this is usually temporary due to measures taken during the procedure.
“GAE is a suitable bridge therapy to knee replacement in patients with osteoarthritis and provides an alternate option for patients seeking pain relief,” he said. “It is important to delay knee replacement for younger patients, as they will need another replacement in approximately two decades. Pushing back replacement with other treatments can reduce the total number of surgeries a patient must undergo in their lifetime.”
To refer a patient for Genicular Artery Embolization at ChristianaCare, please call 302-733-5625 or complete the form at the bottom of this page.
ChristianaCare’s Advanced Heart Failure Clinic—part of the Center for Heart and Vascular Health—specializes in surgical and nonsurgical treatments for patients dealing with the most challenging aspects of refractory heart failure.
“We have the first and only advanced heart failure center in the state, and have been Joint Commission−certified since 2013,” said Ray A. Blackwell, M.D., the chief of cardiac surgery at ChristianaCare’s Center for Heart & Vascular Health and also the W. Samuel Carpenter, III, Distinguished Chair of Cardiovascular Surgery. “We provide care for patients with advanced heart failure who have very limited options.”
Without specialized care, an overwhelming majority of these patients may not survive one year, Dr. Blackwell said.
“The Advanced Heart Failure Clinic provides comprehensive evaluation of a patient,” added Neeta Tripathi, M.D., the interim director of Advanced Heart Failure at ChristianaCare. “We determine if they are on the right medications at the correct doses, and decide whether they need advanced therapies.”
Determining which strategy will best address these patients’ needs is a complicated process. Options typically include hospice care, intravenous medications, transplantation and the use of mechanical pumps such as a left ventricular assist device (LVAD).
An LVAD can be a lifesaving choice for both individuals who are waiting for heart transplants, and those for whom transplant is not an option. Currently, ChristianaCare is the only health system in Delaware that offers the LVAD.
“Sometimes LVAD implantation is done as destination therapy, which means that it will be used for long-term, lifelong support,” Dr. Tripathi said. “Other times, an LVAD may be used as a bridge to either transplant or recovery.”
“Transplant is a limited option based on organ availability, blood type, body size, social habits and other criteria. Some patients are waiting for a transplant but need an LVAD to bridge them to the transplant,” Dr. Blackwell added.
LVADS are commonly used as a bridge to transplantation in patients who are smokers, and need to have quit tobacco for a period of six months before being eligible for transplant. Similar situations can occur for patients who have a substance abuse disorder.
“There is also typically a weight cutoff at most transplant centers, meaning that people who are obese are not eligible for transplant,” Dr. Tripathi said. “Combining dietary changes and the use of medications such as GLP-1 [glucagon-like peptide-1] agonists allows most of these patients to lose the necessary weight in order to become eligible, and an LVAD can be used as a bridge to transplant in these individuals.”
For patients who may not be eligible for mechanical devices, the Advanced Heart Failure Clinic offers a dedicated, multidisciplinary care team which will be customized to fit each person’s individual needs.
“We have coordinators, cardiac surgeons, advanced practice providers and heart failure cardiologists on call 24 hours a day, seven days a week, 365 days a year,” Dr. Blackwell said. “This allows our patients with end-spectrum heart failure to stay in the state for their care, and to always have access to a multidisciplinary team.”
To refer a patient for Advanced Heart Failure at ChristianaCare, please call 302-733-1663 or complete the form at the bottom of this page.
A newly unveiled program at ChristianaCare is aiming to increase connectivity between patients and their healthcare team, and shift aspects of care so they can take place where people are most comfortable: in their homes.
“At ChristianaCare, we have six aspirations, and one of them is keeping people healthy at home,” said Sarah E. Schenck, M.D., the executive director of ChristianaCare’s Center for Virtual Health. “The development of this program is all part of this system work around the concept that home is the new venue of care, and that things that typically had been done in a doctor’s office or hospital can be done safely at home—sometimes with even better results.”
The Remote Patient Monitoring program uses connected technology in order to allow experts at ChristianaCare to easily and frequently monitor patients’ biometrics, such as pulse and blood pressure. Data are uploaded using the patient’s mobile device and seamlessly sent to the individual’s care team members, allowing for adjustments to be made far in advance of scheduled office visits.
“This type of high-frequency, low-intensity care helps us stay connected to the patient literally on a daily basis,” Dr. Schenck said.
Much of the impetus for the program came from discussions within the Center for Virtual Health regarding how to improve health equity and address the changing needs of modern consumers.
“When we think about health equity with regards to blood pressure management, we think about the ability to access visits, to manage and maintain blood pressure, health literacy, and the many other barriers one might encounter as a patient,” said Marshall Hawkins, the administrative director at the Center for Virtual Health. “Then we add this into our disparate populations, specifically our Black and Brown communities, which have historically demonstrated higher blood pressure with lower ability to manage it through visits and medications.
“Published literature would suggest the best way for us to approach these issues is to create a personalized approach to care, just like we do in all avenues of care, so that we can deliver care in a way that creates systems of support,” Hawkins added. “This program does that by working with health messages and reading a daily routine where there is a back-and-forth between the care team and the patient.”
Dr. Schenck agreed that access to healthcare is a critical challenge, and that it can be difficult for many patients.
“At ChristianaCare, we have a growing aging patient population with increasing levels of chronic conditions that need to be managed,” she said. “This means that we’ve needed to think in different ways in order to manage patients without needing to rely on office visits.”
The program also addresses changes in how consumers have come to think of healthcare and what they expect to receive from the health systems in their community.
“We have come to expect a level of care in other industries where just about anything can be quickly and easily delivered to your door,” Dr. Schenck said. “We need to meet our patients where they are.”
Home monitoring also can allow for more consistent data, which can paint a more complete picture of a person’s state of health.
“As physicians, we often base our clinical decisions on one or two data points when a patient comes into the office,” Dr. Schenck said. “This is a tiny window into what their blood pressure is doing day after day. More data points allow us to evaluate a patient’s health over time in their native environment, allowing us to make clinical decisions based on more accurate data.”
From a cardiology perspective, home care can be particularly beneficial for patients with heart failure.
“While many cardiac diagnoses require an acute care hospital, heart failure lends itself well to being managed at home, with both dietary counseling and monitoring conducted by Remote Patient Monitoring support staff,” said Audrey A. Sernyak, M.D., the associate section chief of cardiology at ChristianaCare, and medical director of ChristianaCare Cardiology Consultants. “This can be a huge help for our patients.”
“Receiving care in the home can be significantly more comfortable for a patient, and this remote monitoring can allow us to keep certain patients from needing to come to the hospital,” said Neeta Tripathi, M.D., the interim director of Advanced Heart Failure at ChristianaCare. “This can help to cut down on unnecessary hospital admissions and reduce the risk of complications such as hospitalacquired infections.”
Overall, the program is intended to increase the level of care for these challenging patients, while reinforcing ChristianaCare’s dedication to implementing next-generation healthcare.
“This is but one of many virtual support tools that we are using to try to keep our patients’ health at home, rather than in the hospital,” Dr. Sernyak said.
To refer a patient for Cardiology at ChristianaCare, please call 302-623-1929 or complete the form at the bottom of this page.
Founded in 2018, the Advanced Lipid Clinic at ChristianaCare offers a home for patients who have difficulty managing high cholesterol, as well as for individuals dealing with complex lipid disorders.
“We get referrals from cardiologists, vascular specialists, endocrinologists and primary care physicians in the area who have patients with challenging lipid disorders,” said Stephen Meng, M.D., a preventive cardiologist at ChristianaCare. The Advanced Lipid Clinic offers expertise for patients who have difficulty tolerating statins, who are at high risk for heart disease and stroke, and who have rare genetic lipid disorders, such as familial hypercholesterolemia, he added.
“Many of the patients we see are people who need more aggressive management,” said Myrna Sutera, AGACNP-BC, MSN, a nurse practitioner who specializes in cardiovascular disease and lipid management. “They may already have heart disease, or are at high-risk for recurrent events that need aggressive lipid lowering. We’re the only lipid clinic in Delaware, so before we were established patients would have to travel to Philadelphia, Baltimore or other locations in order to receive specialty lipid management.”
Both Dr. Meng and Ms. Sutera are board-certified by the American Board of Clinical Lipidology (ABCL) as Certified Lipid Specialists (CLS). There are only a few providers in Delaware who hold this board certification.
As new therapies are developed, Dr. Meng, Ms. Sutera and their colleagues are working to incorporate these advances into their practice.
“Statins have been the mainstay of treatment for nearly 40 years, yet there are people who can’t tolerate them due to side effects and other reasons,” Dr. Meng said. “In recent years, there have been multiple new medications that are geared toward treating LDL [low-density lipoprotein] levels, particularly in those who either can’t tolerate statins or whose numbers are not at goal on maximally tolerated statins.”
These statin alternatives include oral bempedoic acid (Nexletol, Esperion Therapeutics), evolocumab (Repatha, Amgen) injection, alirocumab (Praluent, Regeneron) injection and inclisiran (Leqvio, Novartis). Additionally, in December 2024, the FDA approved olezarsen (Tryngolza, Ionis Pharmaceuticals), the first treatment for adults with familial chylomicronemia syndrome (FCS), which is a rare condition that causes extreme levels of triglycerides in the blood.
“The problem with these folks is they are at risk for pancreatitis, which usually ends up with them needing to be hospitalized,” Dr. Meng said. “For years we didn’t really have good ways to treat these patients. The old drugs weren’t really effective for these people with very high triglycerides.”
In the coming years, it is likely that medications will be approved to treat lipoprotein(a), which, in high levels, has been implicated in cardiovascular disease risk, he added.
As the Advanced Lipid Clinic expands, Ms. Sutera noted the importance of educating patients and physicians in Delaware regarding their offerings and the patient types who are best suited for referral.
“The most appropriate patients for the Advanced Lipid Clinic would be those who have family history of high cholesterol, heart disease or stroke and those who have a genetic condition or complex lipid disorder and are statin-intolerant or people who have already had a cardiac event since they are at a higher risk,” she said.
To refer a patient to the Advanced Lipid Clinic at ChristianaCare, please call 302-623-1929 or complete the form at the bottom of this page.
At ChristianaCare’s Center for Heart & Vascular Health, recent realignments have strengthened the multidisciplinary approach used to care for critically ill patients in both the cardiac (CICU) and cardiac surgery (CVICU) intensive care units.
“The CICU had historically been a place where all cardiologists could admit patients and be the attending physician of record,” said Sandra A. Weiss, M.D., the medical director of the CICU at ChristianaCare. “From a learning perspective, this was an inefficient system because there wasn’t a single touchpoint provider who owned the care of all the patients in the unit at a given time.”
As a result, she added, it was challenging to provide uniform care to all patients over the course of time.
To address this, ChristianaCare hired a team of full-time cardiac intensivists, specialists boardcertified in both cardiology and intensive care. This has allowed the team to effectively provide intensivist coverage 24/7, 365 days a year. Additionally, the change allowed for the CICU to move to a closed-unit model where patient care is managed uniformly by a single cardiac intensivist at any given time.
“The benefit of this approach is that one person is managing the whole unit for seven days at a time,” Dr. Weiss said. “This approach has been studied and is proven to reduce cost of care and length of stay and results in safer care.”
Planning for this change in the structure of the CICU took place over a period of three years, which allowed time to get buy-in from all key stakeholders and reassure referring physicians that their patients were in the best hands, according to Dr. Weiss.
“Because this model germinated over the course of three years, our independent providers felt comfortable that the care of the patients was going to be left in the hands of people who are specifically expert in the care of these critically ill patients,” she said. “We have worked very hard to make sure that communication between the intensivist practice and independent providers is robust so that everyone feels like they are in the loop regarding care of patients they may have known for years. In addition to the team of advanced practice clinicians and cardiology fellows who provide patient coverage, the cardiac intensivists add another layer to the care of patients in the CICU.”
“The CICU and CVICU handle a variety of medical and surgical conditions that require immediate attention, some of which arise when the cardiac surgeons are in the operating room,” said Ray A. Blackwell, M.D., the chief of cardiac surgery at ChristianaCare’s Center for Heart & Vascular Health, who is also the W. Samuel Carpenter, III, Distinguished Chair of Cardiovascular Surgery at Sidney Kimmel Medical College of Thomas Jefferson University, in Philadelphia. “The cardiac surgery intensivist has made the care more streamlined, standardized, immediate and efficient.”
Nawar Al-Rawas, M.D., a cardiac anesthesia intensivist and the medical director of extracorporeal membrane oxygenation and the CVICU at ChristianaCare, agreed that the introduction of intensivists to the CVICU last summer has helped by allowing surgeons to focus more on their work in the OR.
“One of the big missions we have is to ensure that there is always someone available 24/7 from the intensive CVICU who can immediately address any concerns, can physically come to a patient’s bedside or can alert cardiac surgeons, cardiologists or other disciplines as needed,” he explained. “Both CVICU and CICU are complex environments with challenging cases and high acuity. So, having a sense that experts are available continuously will enhance patient care, communication and satisfaction.”
This tailored approach to care, and the ability to customize it as needed for individual patients, is what sets the Center for Heart & Vascular Health’s CVICU and CICU apart from services offered by most hospitals and health systems.
“The multidisciplinary group can tailor itself to the patient’s needs,” Dr. Weiss said. “Not many hospitals offer that level of attention, especially with the acuity of the patients that we take care of.”
A novel procedure that treats resistant hypertension by reducing nerve activity in the renal artery is becoming available at ChristianaCare, which was a participant in the research trials that led to FDA approval of the devices used in the approach.
The procedure, renal denervation, is a minimally invasive approach that uses a catheter to send ultrasound or radiofrequency (heat) energy to the vessels that supply blood to the kidneys. That energy destroys renal nerves without damaging the arteries, leading to a drop in blood pressure.
“It’s long been known that blood flow to the kidney has a lot to do with the control of blood pressure in general,” said ChristianaCare cardiologist Neil Wimmer, M.D. “A number of the medications we use to treat hypertension work either on the kidney or kidney hormones. For more than a decade, research has been exploring whether we can control blood pressure by changing nerve signaling in or to the kidney.”
The renal denervation program at ChristianaCare engages a multidisciplinary team of specialists that includes cardiovascular surgeons and vascular and interventional radiologists, among others. Within the past year, two renal denervation devices—Paradise (Recor Medical) and Symplicity Spyral (Medtronic)— have been approved by the FDA, after a series of clinical trials demonstrated that they could significantly reduce blood pressure. The first device is a balloon-based device that is inflated within the main renal artery, allowing surgeons to ablate the area to improve blood flow; the other is a spiral catheter that is advanced above the main renal artery up to three to five distal arteries, which are then ablated, according to Daniel Leung, M.D., vascular interventional radiologist at ChristianaCare.
Both procedures can cause pain, and are performed under general anesthesia, but they achieve excellent outcomes, he added.
“On average, we can say that doing this procedure with one of these systems leads to a drop in systolic blood pressure of around 5 to 10 mm Hg from baseline, which is equivalent to about one blood pressure drug in the multidrug cocktail that most patients with hypertension usually take,” Dr. Wimmer said. “We do not yet know how long the benefit will last, but based on study follow-up so far, we can safely say that, in multiple studies involving multiple patients, there has been sustained blood pressure reduction for at least three years.”
Renal denervation is performed using image guidance and is minimally invasive. Image guidance ensures the energy accurately targets the nerves without damaging the surrounding arteries. It also helps guide the catheter used in the procedure, Dr. Leung said.
“Image guidance is vital for renal denervation to be effective,” he said. “Our team has expertise in the technical, procedural aspect, since we treat patients with renal vascular hypertension, typically with stents. So, with this procedure, we’re in the surgical suite, working with cardiologists to achieve optimal outcomes with the procedure. Renal denervation can have a significant impact on patients with uncontrolled hypertension.”
“The device is not particularly large, and it is very similar to those used in other procedures that we already do routinely in our interventional cardiology and cardiac catheterization labs,” Dr. Wimmer added. “It takes approximately two hours under local anesthesia, and most patients are able to have the procedure and go home the same day. If someone has a very high absolute risk, even if you lower their blood pressure by just 10%, that’s much more significant than lowering it by 10% in someone with a very low absolute risk.”
The procedure carries a very low risk for complications; rare complications include bradycardia, leaking in the artery (pseudoaneurysm), renal artery stenosis and tears in the renal arteries. Some patients may not be candidates for renal artery denervation if they have issues with blood flow to their kidneys, significant kidney dysfunction or significant peripheral artery blockages.
“While this is not a magic treatment for resistant hypetension, it’s a significant contributor to our ability to get blood pressure under control, particularly for people who may have a difficult time with taking multiple medications due to availability, drug–drug interactions and the complexity of the regimens,” Dr. Wimmer said. “Since hypertension is associated with stroke, heart attack and kidney disease, getting it under control can have a major impact on a person’s health outcomes.”
Although the studies of renal artery denervation have demonstrated success across a range of hypertension levels, from mild to moderate to severe and even resistant hypertension, at ChristianaCare, the procedure is initially being offered primarily to patients at high cardiovascular risk for whom overall blood pressure reduction would have particular benefit. It’s estimated that nearly 8 million people in the United States have resistant hypertension. People with resistant hypertension are significantly more likely to experience death, heart attack, congestive heart failure, stroke and/or end-stage renal disease.1
“For these patients, they get more bang for the buck in treating high blood pressure, because their risk can drop more,” Dr. Wimmer said. “If we can prevent some of these complications with the help of this procedure, that will be a great step forward. We are very excited to be able to offer renal artery denervation as part of the suite of options for treating our patients with high blood pressure. It is not a miracle cure, because hypertension is a complicated problem. Even with this technology, we expect most people to still require drug therapy and all the lifestyle and other interventions that reduce cardiovascular risk long term. It’s part of what we believe to be the foundation of comprehensive cardiovascular care for the future—but part of the foundation, not the whole house.”
To refer a patient for Renal Denervation at ChristianaCare, please complete the form at the bottom of this page.
References
1. BMC Nephrol. 2019;20(1):138.
A partnership between ChristianaCare cardiologists and oncologists is enhancing heart care for breast cancer patients receiving high-risk chemotherapy.
The Cardio-Oncology Program was established five years ago by physician leaders from the health system’s Women’s Cardiology Clinic and the Helen F. Graham Cancer Center & Research Institute to prevent and effectively treat cardiotoxicity in breast cancer patients on chemotherapy. The program also sees women with lymphoma and ovarian and uterine cancers who receive high-risk chemotherapy and need to be monitored for cardiotoxicity.
“Through the program, cardiologists closely monitor women before, during and after chemotherapy with drugs known to cause cardiotoxicity,” explained Audrey A. Sernyak, MD, Associate Chief of Cardiology and one of the clinic cardiologists who along with noninvasive cardiologist Robin A. Horn, MD, was instrumental in developing the partnership. “The goal is to protect patients’ heart health and optimize their cancer care in collaboration with oncologists.”

There is a growing need for ongoing patient surveillance because of the emergence of new chemotherapy drugs that can cause cardiotoxicity, and because breast cancer survivors are living longer and dealing with the lasting effects of treatment, according to Dr. Horn.
“Fortunately, there are a number of actions cardiologists can take to address the complication, including prescribing medications, recommending adjustments to care plans and suggesting lifestyle modifications,” Dr. Sernyak noted. “Sometimes, chemotherapy can even be paused to give the heart time to recover from cardiotoxicity, and then resumed so treatment can be completed.”
At ChristianaCare, the Cardio-Oncology Program is structured with patient convenience and efficiency in mind. When women receive a referral, clinic staff schedule appointments for them to have an echocardiogram and see a cardiologist within one week to avoid any delay in the start of their chemotherapy.
“The appointments happen on the same day,” Dr. Sernyak explained. “First, they have their echo and immediately afterward they meet with a doctor to review their results and discuss appropriate next steps based on the findings.”
Patients then return for follow-up testing every three months and appointments with a cardiologist every six months throughout their chemotherapy regimen and beyond to evaluate their heart function and identify and treat any cardiotoxicity that may develop, Dr. Horn added.
Program cardiologists keep referring physicians closely up to date on patients’ status through the ChristianaCare electronic medical record system and personal consultations.
“We emphasize building strong, collaborative working relationships,” Dr. Sernyak said. “The oncologists appreciate the expertise our cardiologists bring to the care team, which enables them to focus on treating breast cancer. It’s a partnership designed to deliver an exceptional patient experience and achieve the best possible medical outcomes.”
To refer a patient to the Cardio-Oncology program at ChristianaCare, please call (302) 623-1929 or fill in the form on this page.
At least 6.5 million people aged 40 years and older in the United States have peripheral artery disease (PAD). Like many chronic cardiovascular conditions, the prevalence of PAD increases with age: By age 70, more than 10% of men and nearly 10% of women will be diagnosed with the disorder. By age 80, those figures increase to more than 25% and 20%, respectively.1
PAD’s most severe manifestation is critical limb ischemia (CLI). Recent research indicates that as many as 1 in 4 people who develop CLI will have an amputation within one year of their diagnosis.2 A 2021 study found that the rate of hospital admissions for CLI increased from 0.9% to 1.4% between 2011 and 2017, while PAD admissions nearly doubled, going from 4.5% to 8.9%, over the same period.3
“With the epidemic of obesity and diabetes, PAD and CLI are increasing,” said Daniel Leung, MD, vascular interventional radiologist and fellowship program director at ChristianaCare, where about 500 endovascular revascularization procedures are performed annually. “Our PAD service at ChristianaCare is very busy, and we have a wealth of expertise in the clinical management of these patients as well as endovascular procedures to save limbs threatened by CLI, performed in our state-of-the-art angiography suites.”
Both the equipment and surgical techniques used to manage PAD and CLI are rapidly evolving. One of the most novel therapies now available at ChristianaCare is transcatheter arterialization of deep veins (TADV), which is used to treat patients with the most severe CLI who have run out of revascularization options. TADV is designed to reestablish blood flow by diverting arterial flow from the tibial artery to deep veins in the foot.
“We connect the vein to the artery and backfill the tissues of the wound to get oxygen to that area,” Dr. Leung explained. “With advances like these, as well as increased awareness among referring physicians to send their patients to specialists like our team if they have PAD, I believe we are making progress in reducing the number of amputations that are done.”
He continued: “This is a rapidly evolving field with lots of innovations and novel devices and, at ChristianaCare, our patients have access to those options, including investigational procedures in clinical trials. We are involved in the development of complex revascularization techniques, such as pedal access and pedal loop revascularization to treat the very small arteries in the foot. Even though this is not generally done that frequently, it is something we do here on a routine basis.”
ChristianaCare was also involved in the trials introducing drug-eluting balloons and drug-eluting stents, which had become common in the treatment of cardiovascular disease, to treat peripheral vascular disease.
“This is now standard of care, but our patients had access to these technologies in trials before they were commercially available,” said Dr. Leung, who also stressed the importance of podiatry and wound care in the management of these patients. “Our team of vascular interventionalists regularly visits our affiliated off-site wound care center to evaluate patients for surgery, as it is more convenient for patients to be seen there.”
The interventional vascular team works closely with ChristianaCare’s team of vascular surgeons and a multidisciplinary group of experts including infectious disease physicians, endocrinologists and nephrologists, as well as the many podiatrists who work in the area. In addition, cardiologist Vikash Rambhujun, MD, has returned to ChristianaCare after a one-year fellowship at Yale University Hospital, where he studied vascular medicine and procedural care of PAD. His work is expected to complement that of the others on the multidisciplinary team.
“We also partner with primary care physicians to raise awareness,” Dr. Leung said. “Many of the patients we see have come into the emergency department with disease that is already quite advanced. By working with primary care and family practice and encouraging them to send patients to us early on, we can improve their outcomes.”
To refer a patient with Peripheral Artery Disease to ChristianaCare, please call (302) 733-5625 or fill in the form on this page.
References
1. CDC. Peripheral arterial disease (PAD). Accessed May 13, 2024. https://www.cdc.gov/heartdisease/PAD.htm#
2. Mustapha JA, Saab FA, Ranger WR, et al. Treatment of peripheral artery disease and critical limb ischemia: an observational Michigan Medicare analysis. J Crit Limb Ischem. 2023;3(2):E56-E63.
3. Anantha-Narayanan M, Doshi RP, Patel K, et al. Contemporary trends in hospital admissions and outcomes in patients with critical limb ischemia: an analysis from the National Inpatient Sample Database. Circ Cardiovasc Qual Outcomes. 2021;14(2):e007539.
ChristianaCare offers prostate artery embolization (PAE) for men with an enlarged prostate—a minimally invasive alternative to traditional surgery.
“Benign prostatic hyperplasia [BPH] is extremely common, affecting more than 50% of men over age 50 and about 90% of men older than age 80,” explained Christopher Grilli, DO, a vascular interventional radiologist.
The condition frequently causes a narrowing of the urethra that interferes with the normal flow of urine from the bladder.
“Prostate artery embolization is an innovative solution to the problem for men who have tried lifestyle changes or medications without achieving satisfactory results, and who would prefer to avoid surgery,” Dr. Grilli noted.
ChristianaCare is the only health system in Delaware that offers the procedure. During PAE, a catheter is inserted through the patient’s wrist or groin and guided by advanced x-ray imaging to the prostate arteries. Tiny beads, or microspheres, are then injected into the vessels, which partially block blood flow and gradually shrink the prostate by 30% to 40%. PAE typically takes one to three hours.
The procedure offers men with BPH many benefits, according to Dr. Grilli.
“The preservation of sexual function is a major factor for men in choosing PAE,” Dr. Grilli said. “Many also prefer the procedure over surgery because it doesn’t involve the insertion of a scope into the urethra and is substantially more comfortable for the patient.”
ChristianaCare closely monitors the effectiveness of PAE by surveying patients before and multiple times after the procedure. The results show 95% of patients report significant improvement in their BPH symptoms.
Dr. Grilli is part of a highly skilled team of four vascular interventional radiologists at ChristianaCare who specialize in performing PAE with the latest equipment and technology. Together, they perform a high volume of the procedures, which translates to greater clinical expertise and better patient outcomes.
“As a doctor, it’s very gratifying to be able to help men regain normal urinary function and experience improved quality of life,” he said.
To refer a patient for Prostate Artery Embolization at ChristianaCare, please call (302) 733-5625 or fill in the form on this page.
Atrial fibrillation, or Afib, is a heart arrhythmia associated with an increased risk for stroke, heart failure and other cardiovascular comorbidities. It is more commonly diagnosed in men and those of advancing age; roughly three-fourths of those with the condition are 65 years or older. Up to 6.1 million people in the United States have Afib, a figure that is projected to reach nearly 12 million by 2030.1
Because of patients’ increased risk, it is imperative to mitigate any structural issues with the heart that can lead to stroke, according to Kevin Tsai, MD, a clinical cardiac electrophysiologist at ChristianaCare.
“The irregular heart rhythm in Afib can cause blood to pool in the left atrial appendage (LAA), a small pouch in the upper left chamber of the heart, which increases the risk of clot formation,” Dr. Tsai said. “If a clot dislodges and travels through the bloodstream to the brain, it can cause a stroke.”
When patients with Afib arrive at ChristianaCare, clinicians assess for symptoms and treat risk factors associated with the condition, including hypertension, heart disease, diabetes, obesity, alcohol/tobacco use and sleep apnea. Patients’ stroke risk is assessed by a score calculated using multiple risk factors, including presence of congestive heart failure, hypertension and diabetes as well as history of stroke and vascular disease, among other factors, according to Dr. Tsai.
Anticoagulants (blood thinners) are traditionally prescribed to reduce patients’ stroke risk. However, in patients unable to tolerate long-term anticoagulants, perhaps due to fall or bleeding risks, ChristianaCare offers occlusion of the LAA, which has been shown to be effective in reducing Afib-related stroke.2
In addition, treatment of Afib focuses on controlling heart rate or rhythm. The aim is generally to control heart rate without converting Afib to a normal rhythm. This treatment is commonly used for patients who tolerate Afib well without symptoms. Rhythm control aims to restore and maintain normal rhythm and is commonly used for patients who have limiting symptoms from Afib.
“Roughly 20% of patients with Afib have no symptoms and, for them, we typically employ the rate control strategy,” Dr. Tsai said. “However, the remaining 80% have symptoms that can greatly diminish quality of life, such as palpitations, shortness of breath and fatigue. Rhythm control strategy is used in these patients to reduce the overall Afib burden by modifying electrical properties of the heart with antiarrhythmic medications and/or catheter-based ablations.”
Although catheter ablation has been shown to be more effective in maintaining normal rhythm, antiarrhythmic medication is currently first-line therapy, according to Dr. Tsai. In patients with Afib that is refractory to antiarrhythmic therapy, catheter ablation can be considered. (Future guidelines may change with recent large clinical trials showing favorable results with the approach; it currently has a class Ia indication with reduction in mortality in patients with heart dysfunction and heart failure due to Afib.)
Generally, the goal of ablation is to disable the cells in the heart that are responsible for triggering and propagating Afib. Two common ablation methods are cryoablation (freezing these cells) or radiofrequency ablation (heating the cells). Both approaches are offered at ChristianaCare, and they can be performed safely and effectively as outpatient procedures.
In cryoablation, electrophysiologists use a balloon catheter to freeze the targeted heart cells, disabling their ability to transmit electrical currents. This procedure can be tricky, however, because if the seal between the balloon, which contains nitrogen refrigerants, and the cardiac tissue isn’t closed, the flow of warm blood can make the procedure less effective, according to Dr. Tsai. The freezing strategy, although mostly safe, can damage nearby structures.
In radiofrequency ablation, electrophysiologists use a catheter to deliver heat to the targeted cardiac cells, rendering them unable to transmit electrical signals. This heating strategy, in rare cases, can also cause collateral damage to nearby structures, Dr. Tsai said.
The most recent advancement in Afib is pulsed-field ablation (PFA), which was approved by the FDA in December 2023 and involves a large electrical current (1 microsecond in duration) that causes cardiac cells to undergo apoptosis. ChristianaCare is expected to begin offering PFA within the next year, and Dr. Tsai believes it will change the treatment landscape of rhythm control for Afib.
“The benefit of PFA is that different tissues in your body absorb the electrical field at different amplitudes,” Dr. Tsai explained. “You can deliver PFA and it will only affect the cardiac cells without adverse effects to nearby structures, including the esophagus, arteries/veins and the phrenic nerve.”
To refer a patient with Atrial Fibrillation to ChristianaCare, please call (302) 623-1929 or fill in the form on this page.
References
1. Colilla S, Crow A, Petkun W, et al. Estimates of current and future incidence and prevalence of atrial fibrillation in the U.S. adult population. Am J Cardiol. 2013;112(8):1142-1147.
2. Moras E, Gandhi K, Yakkali S, et al. Left atrial appendage occlusion as a strategy for reducing stroke risk in nonvalvular atrial fibrillation. Cardiol Rev. 2024 Jul 30. doi:10.1097/CRD.0000000000000757
ChristianaCare’s new multidisciplinary Center for Aortic Health brings together some of the region’s leading subspecialty experts in cardiovascular care, including vascular surgeons, cardiologists, cardiothoracic surgeons, interventional radiologists and others, to centralize the care of patients with aortic disease and improve their outcomes.
New 2024 guidelines from the European Association for Cardio-Thoracic Surgery and the U.S. Society of Thoracic Surgeons, which have reclassified the aorta as an independent organ on par with the heart, lungs and brain, recommend bundling the treatment of the aorta in a separate specialty in close coordination with other specialties.1

“Aortic pathology requires specialized management, and we provide the most optimal care for these patients when we work together seamlessly,” said one of the Center’s co-directors, vascular surgeon Kathryn E. Bowser, MD. “There are cutting-edge developments constantly going on in this field, and a center like this one is needed to give patients the best options.”
Led by Dr. Bowser, preventive cardiologist Stephen Meng, MD, and cardiothoracic surgeon J. Daniel Robb, MBBS FRCS, the Center proactively identifies patients with aortic pathology such as aortic aneurysms and aortic dissection before these conditions become emergent; provides them with the latest in medical, surgical and endovascular management; and maintains ongoing coordinated longitudinal care for months and years afterward. Other patients presenting with life-threatening acute aortic dissection receive emergency lifesaving complex surgery and are similarly followed longitudinally.
“The team at the Center for Aortic Health utilizes a multidisciplinary approach that emphasizes patients’ long-term heart health,” said Dr. Robb, who serves as a co-director of the Center along with Drs. Bowser and Meng. “We also pride ourselves in having expertise and experience with multiple surgical and treatment approaches so that we can truly offer patients the best options for their specific needs. We strongly believe that these various approaches are best used in a multidisciplinary team setting to provide patients with inclusive and optimal care.”
For surgical procedures, the Center offers a state-of-the-art hybrid OR, located in the Gerret and Tatiana Copeland Heart & Vascular Interventional Suites, where both open surgery and endovascular procedures can be performed in the same space, with access to advanced imaging technologies including angiography, ultrasound and CT. It’s the only OR of its kind in Delaware. Within the next year, a second hybrid OR will be constructed, increasing the Center’s capacity to manage complex cases.
Thoracic endovascular aortic repair (TEVAR) and endovascular aortic repair (EVAR) have become the first choice of treatment in many patients with thoracic and abdominal aortic aneurysms, respectively. However, many patients have anatomy that is not suitable for standard TEVAR/EVAR procedures, according to Dr. Robb. Novel endograft devices have made TEVAR/EVAR possible for more patients, and ChristianaCare is recognized by device manufacturers as a high-volume institution with the expertise needed to implant these newer models.
“For example, in 2023, we became the first center in Delaware to implant the GoreÒ TAGÒ Thoracic Branch Endoprosthesis, a novel endograft designed to repair the descending thoracic aorta in cases of aneurysm, transection or dissection,” Dr. Bowser said. “Within the next few months, we will also be offering Gore’s Thoracoabdominal Branch Endoprosthesis, another endograft option that allows us to tailor treatment to a patient’s specific anatomy. These are just two examples of the ongoing developments in the field to which patients in the Center for Aortic Health will have access.”
“Patient selection is clearly key to achieving the best possible outcomes in these procedures,” Dr. Robb added.
Another aspect of this customized care for aortic disease is seen in women.
“We are learning more about aortic pathology in women,” Dr. Bowser noted. “Most existing research had primarily been done in men, but more recent studies demonstrate that we must account for differences not only in vasculature size but other factors that may affect care decisions.”
For example, studies have shown that women have a threefold increase in the risk for aortic dissection or rupture, and acute aortic syndromes, such as aortic dissection, occur at smaller aneurysm sizes in women than men.2
“A 5-cm aneurysm in a woman is much more likely to rupture than a similarly sized aneurysm in a man,” Dr. Bowser said. “Our center incorporates all of the latest research into our decision making to create a personalized treatment plan for each patient.”
It was a very specific decision to name the program the “Center for Aortic Health,” according to Dr. Meng.
“We are not just focused on pathology and surgery,” he said. “Our program is distinguished by a patient-centered focus that aims to prevent catastrophes with education and screening. For example, we have been in discussion with the program at Nemours Children’s Health about transitioning some of their pediatric aortic patients into our care as they reach adulthood. There are familial conditions such as Marfan syndrome, Loeys-Dietz syndrome and vascular Ehlers-Danlos syndrome that can raise the risk of aortic pathology conditions. We believe it is important to have a lifelong care plan, not only for the patient but for their family members who may be affected. The Center for Aortic Health offers our community convenient access to world-class expertise right here in their local area.”
To refer a patient to the Center of Aortic Health at ChristianaCare, please call (302) 733-5700 or fill in the form on this page.
References
1. Czerny M, Grabenwöger M, Berger T, et al. EACTS/STS guidelines for diagnosing and treating acute and chronic syndromes of the aortic organ. Eur J Cardiothorac Surg. 2024;65(2):ezad426.
2. Boczar KE, Cheung K, Boodhwani M, et al. Sex differences in thoracic aortic aneurysm growth. Hypertension. 2019;73(1):190-196.
Transcatheter aortic valve replacement (TAVR) at ChristianaCare is revolutionizing the treatment of severe aortic stenosis in older adults.
“TAVR has almost completely replaced open-heart surgery for these patients over the past decade,” said interventional cardiologist and fellowship program director Erin Fender, MD. Dr. Fender is part of a multidisciplinary team that specializes in performing the minimally invasive procedure for the health system’s Structural Heart Disease Program.
The procedure is used to replace a narrowed aortic valve that is obstructing a patient’s blood flow from the heart to the body. If not treated, aortic stenosis can lead to heart failure and death. Though still relatively new, TAVR is already the most common procedure performed by members of ChristianaCare’s Structural Heart Disease Program, directed by Wasif Qureshi, MD, an interventional cardiologist in the health system.
During the procedure, an interventional cardiologist inserts a catheter in the femoral artery which is then guided into the left ventricle allowing implantation of a biological valve to replace the diseased aortic valve. Once in place, the valve immediately restores healthy blood flow. The entire process typically takes less than an hour.
TAVR offers a number of advantages over surgery, according to Dr. Fender:
“These benefits make the TAVR procedure a safe and effective option for the majority of older adults with serious cases of aortic stenosis, including patients in their 80s and 90s,” Dr. Fender noted. “Our interventional cardiologists do hundreds of procedures a year, supported by cardiac surgeons, cardiac nurses and other professionals with extensive experience in TAVR. This multidisciplinary approach and large number of cases translates to advanced expertise that ensures patients receive high quality care.”
ChristianaCare’s TAVR success rate is 99%, and many large clinical trials have repeatedly demonstrated that the long-term survival rates for TAVR equals that of surgery.
“We’re proud to be Delaware’s leader in performing the procedure,” Dr. Fender said.
At ChristianaCare, patients benefit from a timely and efficient TAVR process. When a patient is referred, a cardiac nurse immediately contacts them to arrange every aspect of their care and address any questions or concerns they may have. The nurse assists the patient in scheduling necessary testing and appointments with an interventional cardiologist and cardiac surgeon—often all on the same day to maximize convenience.
After the TAVR, patients return to ChristianaCare for postoperative checkups and then are seamlessly transitioned back to the care of their local doctor. Through the process, the TAVR team keeps the referring physician informed about their patient, the outcome of the procedure and instructions for follow-up care.
“We strive to develop collaborative relationships with doctors by providing thorough communication and being available for consults when needed,” Dr. Fender explained. “By the time the patient meets with me or one of my colleagues, we’ve already reviewed their testing results and are prepared to recommend a course of action, including scheduling their procedure, if appropriate. All of this typically happens within just a few weeks. It’s a well-coordinated pathway focused on delivering an excellent patient experience.”
To refer a patient for TAVR at ChristianaCare, please call (302) 733-1507 or fill in the form on this page.