Login
Primary Care Services
Using Antibiotics Safely
Understanding Antibiotics
Using antibiotics incorrectly has led to antibiotic-resistant germs — here’s what you can do to help.
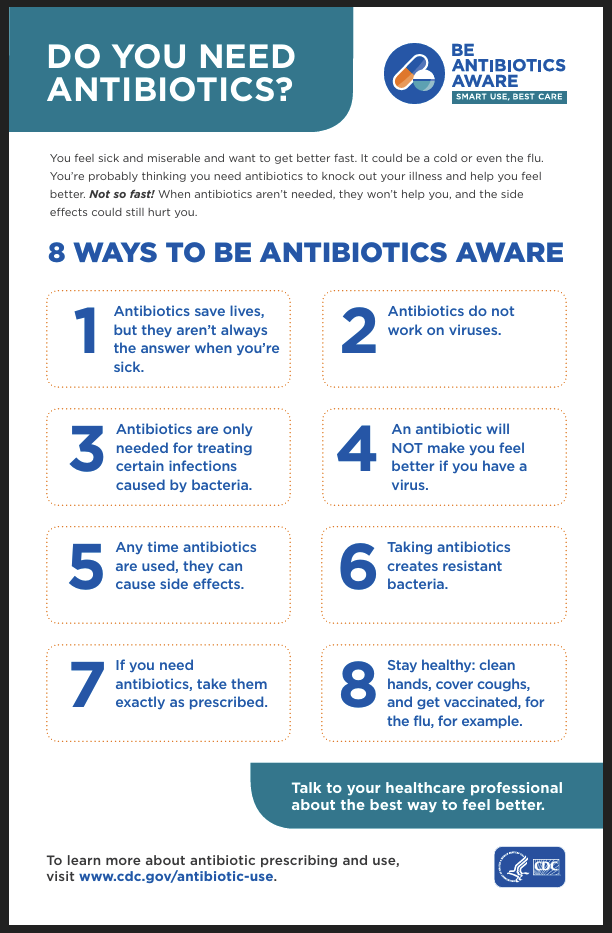
Antibiotics are being used for many unnecessary conditions and viruses, so bacteria are becoming more antibiotic-resistant.
As a result, these medicines are now less effective, causing patients to need different antibiotics that kill a wider range of bacteria. This can lead to more side effects and higher costs. In some rare cases, there may not be any suitable antibiotics available to treat a particular infection.
Therefore, we must use antibiotics appropriately so we can prevent the development of antibiotic resistant infections.
Did You Know?
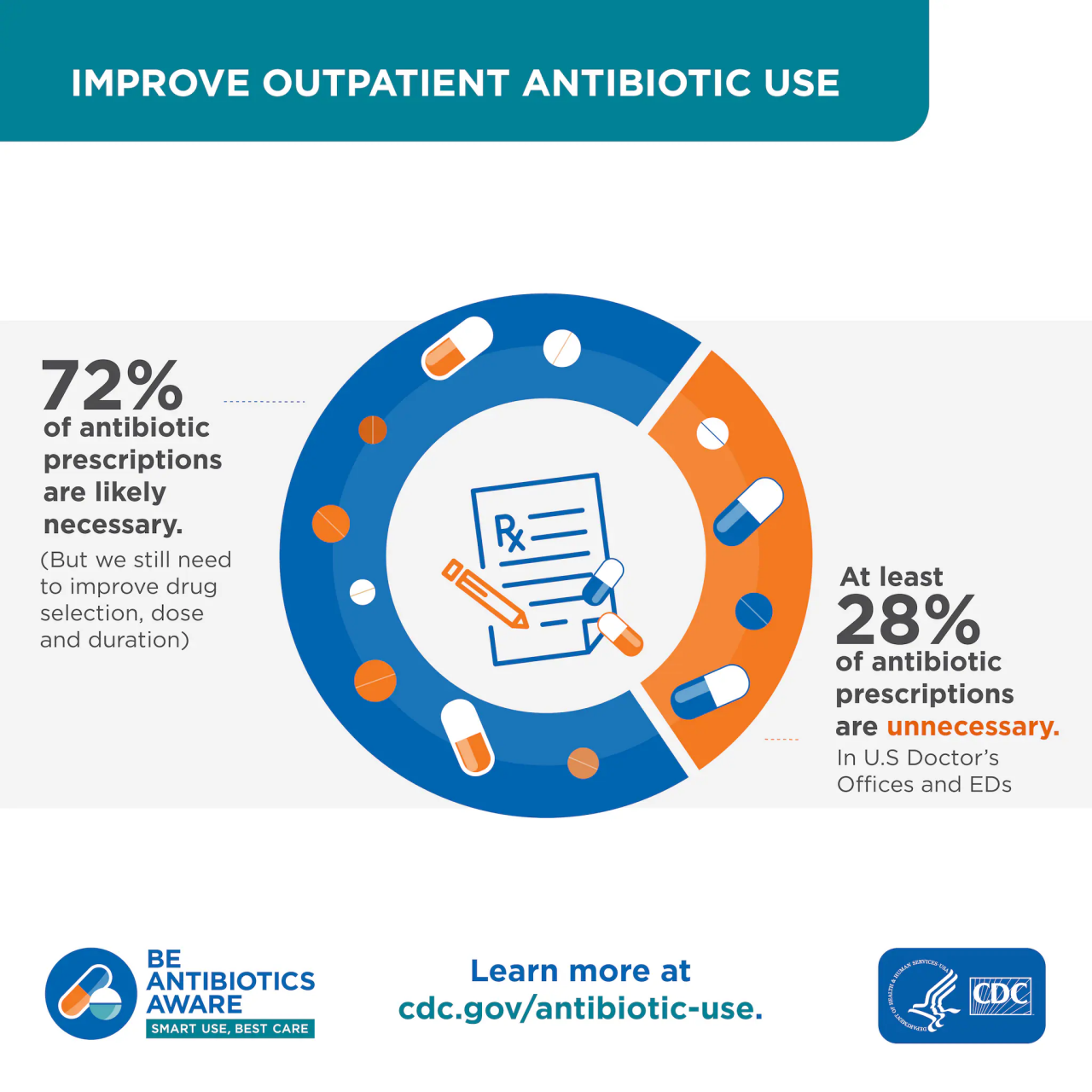
Many Antibiotics aren't needed
Studies show that one-third or more of people receiving antibiotics do not need them, especially for respiratory infections. That’s because you most likely have a virus. You will feel better just as soon without the antibiotic, and you won’t run the risk of having side effects.